|
XVI International
AIDS Conference in Toronto 2006

Aids who it affects 2006
Personal tributes
They are
the names of the dead, neatly handwritten on little white flags.
The 8,000
flags arranged in a field at the south entrance of the Toronto Metro
Convention Centre this week were a personal testament to lives lost to AIDS
each day around the world. It took 40 people and six hours to assemble the
display.
"What we
wanted was to have ordinary folks who care to have their voices heard," said
Lynn Thornton, the executive director of VIDEA, an agency that helped
organize the installation.
Known as
the Community Action on AIDS Project, the Toronto exhibition was one of
eight put up across Canada.
Above the
image of a crying face one caption read: AIDS Doesn't Go Away. Another flag
was simply inscribed: Help.
"Some of
them (are) memories of people who have died, some of them things people
would like to have done here," Thornton said.
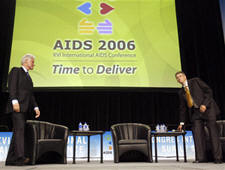
Conference
Theme: Time to Deliver - 13/08/2006
The AIDS 2006 Conference theme, Time to Deliver, underscores the continued
urgency in bringing effective HIV prevention and treatment strategies to
communities the world over. Twenty-five years after the first reports of
what was later to be known as AIDS appeared in the CDC’s Mortality and
Morbidity Weekly Report, the magnitude of this epidemic demands increased
accountability from all stakeholders to fulfill their commitments, be they
financial, programmatic or political.
While additional resources and continued scientific research are critical to
an effective global response, the theme recognises that the scientific
knowledge and tools to prevent new infections and prolong life among those
living with HIV/AIDS already exist, even in the poorest settings. The
challenge at hand is to garner the resources and the collective will to
translate that knowledge and experience into broadly available HIV treatment
and prevention programs.
The International AIDS Conference exists for exactly these reasons. It is
one of the most important gatherings for the release and discussion of key
scientific developments in the fight against HIV/AIDS.
AIDS 2006 will bring together the movement of people responding to the
HIV/AIDS epidemic to share their lessons and together stake out the road
ahead. In doing this, the Conference directly affects the lives of those
living with and affected by HIV/AIDS. AIDS 2006 is a catalyst for change.
They have
different styles, different backgrounds, and they appeal to vastly
different parts of the population. Yet they have at least one thing in
common: Each seems to have made personal the morale-crushing battle
against the scourge of HIV and AIDS. In the process, they have become
among the world's most influential voices as the lethal disease rages in
its 26th year.
Consider
some of the personalities who have enlisted in the fight: There's Bill
Gates, the world's richest man, and Warren Buffett, his closest rival for
the title. There's movie star Richard Gere, who has proven equally adept
at navigating leading Hollywood roles and symposiums at World Economic
Forum gatherings. (In the 1993 TV movie And The Band Played On,
Gere became one of the first movie stars to openly tackle the subject of
AIDS.)
There's
also the likes of Helene Gayle, a one-time leader of the U.S. Centers for
Disease Control who went on to work alongside Gates as a tireless advocate
for women's rights relating to HIV and AIDS. (At a time in the mid-'80s
when some doctors refused to treat AIDS patients and some hospital staff
would leave meals for AIDS patients on the floor outside their hospital
rooms, Gayle championed AIDS-related research even as colleagues urged her
to avoid involvement because the virus was an "oddball disease" that would
peter out in a few years.)
While
others merit mention — including University of Toronto bioethicist Dr.
Peter Singer and Canadian singer Sarah McLachlan, one of the artists most
active in raising AIDS awareness — much optimism in recent days is
connected one way or another to Gates, who seems to have a hand in causes
ranging from rampant infectious diseases such as AIDS, malaria and
tuberculosis to both first- and third-world education. There's no debating
the fact that Gates, the founder of computer juggernaut Microsoft Corp.,
is doing more in the quest to eradicate the virus that causes AIDS than
anyone else these days. His charity, the Bill and Melinda Gates Foundation,
last year alone gave away $1.3 billion (U.S.) and has, for better or worse,
bolstered ties to groups like the World Health Organization, the Global
Fund to Fight AIDS, malaria and tuberculosis, and a hodgepodge of the
world's leading medical researchers.
Then
there are the ties Gates seems to have made to former U.S. president Bill
Clinton, who might not have Gates's financial clout but no doubt has an
impressive Rolodex of his own.
Gates has
made a pledge to help finance Clinton's own charity, and the two, together,
will share the podium at this week's XVI International AIDS Conference in
Toronto.
Philanthropy experts contend that Gates's influence goes beyond his
ability to help prop up non-profits. When he contributes to a cause, it
seems be a catalyst to generate more donations.
Says
Harvey Dale, director of the National Center on Philanthropy and the Law
at New York University: "It's like a contribution from Gates is like a
good housekeeping seal of approval."
That
seems to have been the case for Buffett, whose contribution will allow the
Gates Foundation to more than double its annual giving to roughly $3
billion a year.
To be
sure, with Gates and Buffett presenting a united financial front in the
fight against HIV and AIDS, there are still reasons for caution. Some
infectious-disease experts worry that some governments, seeing the
billions committed by the pair, may decide to pare spending related to the
disease.
Nevertheless, as worldwide scrutiny of HIV and AIDS continues to grow —
this week's AIDS conference in Toronto is expected to attract up to 22,000
delegates, more than 10 times the 2,100 scientists who attended the first
such gathering in 1985 in Atlanta — Gates, Buffett, Gayle and others are
taking centre stage in AIDS-related research, using money and moxie,
charisma and connections, to fight the virus.
Ottawa promises
cheap drugs - Health minister decries lack of aid, But current law
prevents action - Aug. 14, 2006
The federal health minister wants Canada to keep its promise of
supplying cheap AIDS drugs to Africa and is seeking advice on
changing legislation that is hindering the flow of life-saving
medication. "If we can put a man on the moon, we can solve this
issue," said Tony Clement of Canada's Access to Medicines Regime,
which, ironically, was designed to boost the Canadian production
of generic drugs for poor countries. The problem, say critics, is
that Canada based its law on an already complicated framework
designed by the World Trade Organization, and muddled it further
when implementing it into national law. To date, not a single pill
has been exported and not a single patient has benefited from the
Canadian law, which was passed two years ago. "Obviously the
legislation isn't working," said Clement, while attending an
international nurses forum in Toronto on the weekend. In the days
leading up to last night's opening in Toronto of AIDS 2006, the
16th international conference on AIDS — the theme of which is
"Time to Deliver" — activists have been extremely critical of
Canada's record. Clement said he has sought advice from
organizations such as Doctors Without Borders and the Canadian
HIV/AIDS Legal Network, as well as Stephen Lewis, the UN's special
envoy for AIDS in Africa, on how to make the law work.
"We
have failed lamentably," said Lewis. "It's almost unbelievable
that two governments — one Liberal and one Conservative — can't
get a single pill to Africa." Lewis said Clement pressed him "fairly
hard" for advice on Saturday on how to get the drugs flowing. The
answer, said Lewis, is to issue compulsory licences to generic
pharmaceutical companies that would allow them to make drugs
without the patent holder's permission. Currently, legislation
stipulates the drug's patent holder and the generic company
planning to reproduce the drug must negotiate at least 30 days
before asking for a compulsory licence. But there is no time limit
on how long talks can last.
"What's
wrong with these governments?" asked Lewis. "In truth, the
minister of health and minister of industry have all the power in
the world to issue a compulsory licence and get the generic drugs
that Canada promised to Africa at prices that Africans can afford
and will save, ultimately, millions of lives."
One of the companies currently caught in the legislation is Apotex
Inc., which has developed the generic Apo-triAvir, but is locked
in negotiations with the patent holder, GlaxoSmithKline.
"This
is not rocket science — a government has great power," said Lewis,
adding that Clement seemed genuinely interested in doing what he
could. But then again, said Lewis, he had a similar conversation
with the minister three months ago and nothing came of it.
Richard Elliott, deputy director of the Canadian HIV/AIDS Legal
Network, said he and Doctors Without Borders met three of
Clement's advisers last Thursday.
During the hour-long meeting, both organizations tried to hammer
home the point that Canada needs to introduce a more direct and
streamlined mechanism.
"There
are a number of problems with the (WTO) framework and the Canadian
legislation," said Elliott. "But at its core, it's got the process
backward."
Melinda Gates, in Toronto for AIDS 2006 with her husband to
represent the Bill and Melinda Gates Foundation, said yesterday
getting drug companies to lower their prices so more drugs can
make it out to impoverished African nations isn't really an issue
any more.
"The issue now is how do we retain enough personnel in these
countries to help administer and deliver the drugs on an ongoing
basis," she told reporters. "And that cost is still very high."
At a press briefing yesterday, Clement said Canada is doubling its
investment in its national fight against AIDS from the current $42.2
million to $84.4 million by 2008. However, this is not new money —
the original announcement was made in December 2005.
Internationally, Canada has committed $800 million in the present
and as for the future, he hinted an announcement could be
forthcoming.
The fight to get a better system to deliver generic HIV drugs
dates back to Aug. 30, 2003, when negotiations among WTO members
resulted in a landmark decision that allowed generic versions of
patented drugs to be copied under compulsory licence and exported
to developing nations.
According to the decision, a generic producer must negotiate a
tentative contract with a developing country to supply a certain
product in a certain quantity at a certain price. Based on that
agreement, the country must send a notification to the WTO
declaring its intention to import drugs and the generic company
must negotiate with the patent holder for a voluntary licence. If
those talks fail, then the generic producer must apply for two
compulsory licences — one in its home country and one in the
country where the drugs are destined if they're protected under
patent there.
"Each
of these steps is time-consuming and holds no guarantee of
success," reads a report by Doctors Without Borders that will be
presented at the conference.
In
September 2003, Canada announced it would implement the WTO's decision and
in May 2004 it passed the Jean Chrétien Pledge to Africa act, which has
since been renamed Canada's Access to Medicines Regime. But it topped its
legislation with additional requirements that made it even tougher for
generic producers to get drugs out.
For
instance, since negotiations over voluntary licensing between generic
companies and patent holders must last at least 30 days, it is tough to
discern when talks are simply stalled or have broken down. Also, the law is
limited to a list of specific medicines in specific formulations. Even if a
generic company makes it through all those hurdles and a compulsory licence
is granted, it is valid for only two years. After that, the entire process
starts again.
At the bare
minimum, said Elliott, Canada needs to get rid of the extra requirements it
added. But that, he warns, would be "sort of like tinkering around the edges"
and not addressing the real problem which is the original Aug. 30, 2003
decision by the WTO to allow copies of patented drugs.
It's
clearly not working, he said, since no one has taken advantage of it. Not
one country has notified the WTO that it plans to import cheaper drugs.
It's an
indication the barriers to accessing the life-saving drugs are simply too
high, said Elliott.
He said he
proposed to Clement's advisers that legislation be enacted that would
automatically grant a compulsory licence to a generic manufacturer.
With that
in hand, the company could negotiate contracts with various countries and
pay royalties to the patent holder based on whatever deals were reached.
Equip women in
fight, Gates urges - Tools needed to prevent HIV infection. Wants leaders,
drug makers to act fast
Bill Gates
wants world leaders and pharmaceutical companies to give women the power to
prevent the spread of HIV by developing drugs that block the transmission of
the virus.
"This could
mark a turning point in the epidemic and we have to make it an urgent
priority," Gates said last night to thunderous applause during his keynote
speech at the opening ceremony of the International AIDS conference at the
Rogers Centre.
"We want to
call on everyone here and around the world to help speed up what we hope
will be the next big breakthrough in the fight against AIDS."
The
Microsoft chairman explained that in many parts of the world, women are at
the mercy of the men in their lives and do not have the right to refuse sex,
let alone sex without a condom.
"No matter
where she lives, who she is, or what she does, a woman should never need her
partner's permission to save her own life," Gates said.
It was a
sentiment echoed by Peter Piot, the executive director of UNAIDS, who said a
"top priority is to immediately double funding for microbicide research and
development."
A
microbicide is a vaginal gel or cream applied prior to sex that will stop
the transmission of HIV, while oral prevention drugs are antiretrovirals
that, taken before infection, may prevent the transmission of HIV.
In a joint
keynote speech, Gates and his wife, Melinda, also called on the audience of
more than 30,000 scientists, advocates and health workers from around the
world to increase global access to HIV prevention and treatment.
"While
there is promising research to report, the world, in my view, has not done
nearly enough to discover these new tools — and I include our foundation in
that assessment," said Gates, referring to the Bill & Melinda Gates
Foundation, which has donated $650 million (U.S.) to the fight against AIDS
— including $500 million just last week.
Last
night's ceremony included speeches by federal Health Minister Tony Clement,
Mayor David Miller, Premier Dalton McGuinty, Governor General Michaële Jean
and conference co-chair Dr. Helene Gayle, as well as musical performances by
Chantal Kreviazuk, Alicia Keys, Barenaked Ladies and Our Lady Peace.
There was
much discussion among them about the simmering controversy over Canada's
failure to get inexpensive generic drugs to poverty-stricken countries in
Africa, as well as the Prime Minister Stephen Harper's absence from the
conference.
Harper's
office has said he could not attend the summit because he is touring Nunavut
in the Arctic.
Comments by
Dr. Mark Wainberg, conference co-chair and director of the McGill University
AIDS Centre, prompted raucous applause and standing ovations from delegates.
"Mr. Harper,
you have made a mistake that puts you on the wrong side of history," said
Wainberg.
"The role
of prime minister includes the responsibility to show leadership on the
world stage. Your absence sends a message that you do not regard HIV/AIDS as
a critical priority. Clearly, all of us here tonight disagree with you."

Money alone 'not enough'
All the
money in the world will not be able to defeat HIV/AIDS unless great strides
are made in preventing new infections — and that can only be achieved by
giving women and other high-risk groups the ability to protect themselves,
Bill and Melinda Gates said on the opening day of the International AIDS
Conference.
At a news
conference Sunday prior to the opening ceremonies, Bill Gates said that
despite growing access to antiretroviral drugs in countries hard-hit by
HIV/AIDS, between four and five million people worldwide will become
infected in the next year.
"I want to
emphasize we're going to have to do a much better job of prevention to stop
the spread of HIV," said Gates, whose foundation just donated $500 million
US to the Global Fund on AIDS. ``We'll never be able to deal with the
numbers of people that would have to go on treatment if we don't make a
dramatic breakthrough in prevention."
The
Microsoft founder said he would call on the world to accelerate research
into microbicides and oral drugs that would prevent acquisition of HIV. "We
hope and expect that this could be the next breakthrough."
Such
measures are particularly important because they would benefit women who now
have to rely on men to agree to abstinence or condom use.
"And that
simply isn't getting the job done," Gates said. "A woman should never need
her partner's permission to save her own life.
"So there's
progress on these but the pace has been too slow."
His wife,
Melinda, stressed the need to use and make more widely available the tools
known to stop the spread of the virus.
"Today
fewer than one in five people who are at high risk for HIV have access to
things like condoms, clean needles, education and testing," she said. "That's
something that simply needs to change
"One of the
things that we fundamentally believe about HIV the more that we've been
involved in this is you have to put the power in the hands of women. That is
going to be the way to change this epidemic."
Bill Gates
and others called on all governments to join the battle against HIV/AIDS
around the world.
"Obviously
the AIDS epidemic is going to require all actors, particularly governments,
to dig deep and make this a high budgetary priority," he said.
"The amount
of money that's required for universal treatment or the things around
prevention far exceed the amount that any individual government, certainly
any foundation, can possibly provide."
Health
Minister Tony Clement agreed that it will take the collective efforts of
people like the Gateses, international advocacy organizations and
governments to wrestle the pandemic to the ground — and the AIDS conference
offers a fresh starting point for that endeavour.
"I can't
imagine another venue, another event around the world that brings together a
more dynamic, a more diverse, a more committed group of people," Clement
said. "We need all of these people — all of their energy, all of their
collective wisdom and all of their passion perhaps most of all.
"I know
that I'll never be able to fully comprehend the absolute devastation that
flows from the human loss associated with this pandemic. But I want you to
know how committed I am and how the government of Canada is committed to
continuing this fight until it is won."
Conference
co-chair Dr. Mark Wainberg, a leading AIDS researcher at McGill University
in Montreal, said "there is no doubt in any of our minds that HIV is the
planet's public enemy number 1. This conference plays such a vital role in
combatting the spread of HIV."
One goal of
the conference is to make sure drugs are available to those who need them
around the world, regardless of ability to pay, he said.
We all
agree. Access to HIV drugs is a right and not a privilege."
But Frika
Chia Iskandar, an HIV-positive woman from Jakarta, told the news conference
that access to treatment is not just about pills — if people don't live
close to medical care, access to treatment also means being able to afford
to get to where the drugs are being dispensed.
As well,
"stigma and discrimination are still happening," she said, noting that a
dentist refused to treat her last year. "It's still there. Nothing much has
changed."
The
conference has brought an estimated 24,000 delegates and 3,000 journalists
from around the world to Toronto for the biggest gathering in the
now-biennial meeting's 21-year history.
Prime
Minister Stephen Harper has said he will not attend the six-day conference
because of other commitments, a decision that has rankled and baffled
organizers, researchers and AIDS activists — not just in Canada but
elsewhere in th world. Instead, Canada is represented by Clement and
Minister of International Co-operation Josee Verner.
Former U.S.
president Bill Clinton, the crown prince and princess of Norway, UN AIDS for
Africa envoy Stephen Lewis, and actors Sandra Oh and Olympia Dukakis are
scheduled to attend.
Conference
workshops and plenary sessions officially begin Monday, and will deal with a
wide range of issues — from scientific research to caring for those with
HIV/AIDS to preventing the spread of the virus, which has killed 25 million
people in the last 25 years and infected about 40 million worldwide.
Virus a weapon in Congo war -
Infected rebels deployed to rape women, children
About
2,000 rebels infected with the deadly HIV virus were conscripted to rape
women and children in the Democratic Republic of Congo in 1998-99 in a bid
to spread the lethal virus, a new report alleges.
The
allegations levelled at the African countries of Uganda and Rwanda are
contained in a report written by McMaster University professor Ed Mills
and Johns Hopkins University professor Jean Nachega that is being
circulated at the 16th annual AIDS conference in Toronto.
The
report includes a copy of a complaint filed by Congo's government in 1999
with the African Commission on Human and Peoples' Rights in the war with
the two countries.
In its
16-page complaint, Congo alleged that "about 2,000 AIDS-suffering or
HIV-positive Ugandan soldiers were sent to the front in the eastern
province of Congo with the mission of raping girls and women so as to
propagate an AIDS pandemic among the local population and, thereby,
decimate it."
Rwanda
and Uganda have each claimed that Congo did not have the right to file a
complaint with the human rights commission.
While
rape has been employed by armies in Africa and elsewhere, this would be
the first instance where soldiers actively tried to spread HIV and AIDS,
Mills said in an interview.
Children
as young as one were raped by the infected solders, Mills said.
"I've
seen war crimes of every possible stripe, but if this is substantiated,
it's a first," said James Orbinski, president and co-founder of aid agency
Dignitas International.
Congo has
been an epicentre for conflict for years. Several non-governmental groups
have said the country has witnessed more deaths due to violence than any
conflict since World War II, mostly through malnutrition. Between 1998 and
2003, some 4 million people lost their lives.
The
United Nations Security Council initially sent troops to Congo, formerly
Zaire, in 1999 to monitor a ceasefire that ended its fight against Uganda,
Rwanda and Burundi.
That UN
deployment was increased in February 2000, but violence has continued in
the West African nation. Mills said the evidence that Ugandan and Rwandan
troops purposefully spread HIV should compel the recently formed African
Court on Human and Peoples' Rights to hear the charges against the two
countries.
African
foreign ministers earlier this year elected judges to preside over the new
human rights court. The court was formed to give victims of war crimes the
chance to seek compensation against governments.
News of
allegations didn't come as a surprise to NGO workers with experience in
sub-Saharan Africa.
Don Kilby,
with the Canada-Africa Community Health Alliance, which supports an
orphanage near the Congo-Ugandan border, said "it's common knowledge over
there that if they don't kill you they can still hurt you by spreading
AIDS and HIV ... so that the country's blood isn't pure any more."
Kilby
said in his group's orphanage, for instance, there's one 4-year-old boy
who was castrated by rebels as an infant.
"They cut
off his penis and testicles, the whole thing so that he wouldn't make any
more Congo babies," Kilby said. "That's the cruelty of war."
Bill and
Melinda Gates opened the conference on Sunday, August 13. Read their
remarks.:
Bill Gates:
Good
evening.
Thank you,
Helene, for that kind introduction, and for everything you’ve done in the
fight against AIDS. Melinda and I are honored to be with all of you here
in Toronto to open the 16th International AIDS Conference.
Melinda
and I have made stopping AIDS the top priority of our foundation. We can
make this commitment — and make it with serious hope of success — because
of the talent and energy of the people here tonight. Whether you are
working to prevent the spread of HIV, caring for people who live with the
disease, or doing scientific research on the virus, we want to say: Thank
you for dedicating your lives to ending AIDS.
Melinda
and I would also like to thank thousands of people around the world who
are an indispensable part of the fight against AIDS. I’m talking about the
people who are participating in clinical trials as we try to find new ways
to treat and prevent HIV. Science can do nothing without their help — and
we want to offer them our deepest thanks and respect.
Tonight,
Melinda and I want to talk about some encouraging signs we see in the
battle against AIDS, and some signs that are more disturbing. But
ultimately, we want to call on everyone here and around the world to help
speed up what we hope will be the next big breakthrough in the fight
against AIDS — the discovery of a microbicide or an oral prevention drug
that can block the transmission of HIV.
This
could mark a turning point in the epidemic, and we have to make it an
urgent priority.
If we can
discover these new preventive tools and deliver them quickly to the
highest-risk populations – we could revolutionize the fight against AIDS.
Melinda
and I returned recently from Africa. We felt a new sense of optimism there
— because the world is doing far more than ever before to fight AIDS. The
Global Fund is active in 131 countries. It gets HIV drugs to more than
half a million people. It provides access to testing and counseling to
nearly 6 million people. It offers basic care to more than half a million
orphans.
The
Global Fund is one of the best and kindest things people have ever done
for one another. It is a fantastic vehicle for scaling up the treatments
and preventive tools we have today — to make sure they reach the people
who need them. That’s why, last week, our foundation announced a $500
million grant to the Global Fund. We’re honored to be a part of their
work.
The
Global Fund is not the only dramatic advance in the world’s efforts
against AIDS. Shortly after the Global Fund’s launch, President Bush
promised $15 billion over five years to fight AIDS, the largest single
pledge ever made to fight a disease. There were a lot of skeptics at the
time, and a lot of them are probably here tonight.
But today,
PEPFAR is supplying antiretroviral drugs to more than half a million
people in 15 countries in Africa, Asia, and the Caribbean. The President’s
Emergency Plan for AIDS Relief has done a great deal of good, and
President Bush and his team deserve a lot of credit for it.
The
expansion of treatment is making a life-saving difference all around the
world. On our trip to Rwanda last month, Melinda and I went to a clinic,
where they showed us a picture of a thin, sickly man, clearly suffering
from AIDS. I was staring at this picture when a healthy, smiling man
walked into the room and said hello. It took me a minute to realize — it
was the same man.
This is
what treatment is doing for more and more people in the developing world.
We have to build on it — by seeking more funding, creating cheaper drugs
with fewer side effects, and designing more practical diagnostics.
At the
same time, we have to understand that the goal of universal treatment — or
even the more modest goal of significantly increasing the percentage of
people who get treatment — cannot happen unless we dramatically reduce the
rate of new infections.
Between
2003 and 2005, with the infusion of funds from Pepfar and the Global Fund,
the number of people in low and middle income countries receiving
anti-retroviral drugs increased by an average of 450,000 each year. Yet
over the same period, the number of people who became infected with HIV
averaged 4.6 million a year. In other words, for each new person who got
treatment for HIV, more than 10 people became infected. Even during our
greatest advance, we are falling behind.
Let’s
consider what this means for universal treatment. Right now, nearly 40
million people are living with HIV. The lowest price for first-line
treatment drugs is about $130 per person per year; in many cases the cost
is much higher. And the cost of personnel, lab work, and other expenses
easily exceeds another $200 per person per year.
That
means — even when you assume the lowest possible prices — that the annual
cost of getting treatment to everyone in the world who is HIV positive
would be more than $13 billion a year, every year. To put that number in
context, remember that Pepfar — an historic expansion in funding —
designates about $1.5 billion a year for treatment.
This $13
billon figure doesn’t count the cost of much more expensive second-line
therapies, which many patients will need. Moreover, these figures assume
no increase in the number of people living with HIV — yet we’re averaging
4.6 million new infections a year.
We need
to do everything possible to bring down treatment costs, and I’m sure we
will make progress there. But even if you take very optimistic numbers,
when you extrapolate 5 to 10 years, you quickly see that there is no
feasible way to do what morality requires — treat everyone with HIV —
unless we dramatically reduce the number of new infections.
The harsh
mathematics of this epidemic proves that prevention is essential to
expanding treatment. Treatment without prevention is simply unsustainable.
We have
to do a much better job on prevention.
Right now,
one of the most widely practiced approaches to prevention is the ABC
program, for Abstain, Be faithful, use Condoms. This approach has saved
many lives, and we should expand it. But for many at the highest risk for
infection, ABC has its limits.
Abstinence is often not an option for poor women and girls who have no
choice but to marry at an early age. Being faithful will not protect a
woman whose partner is not faithful. And using condoms is not a decision
that a woman can make by herself; it depends on a man.
Another
promising approach is male circumcision. One new study found that it could
significantly reduce the spread of HIV. This is exciting — and if male
circumcision truly is effective, we should make it widely available.
But, like
using condoms, circumcision is a procedure that depends on a man.
That isn’t
good enough.
We need
to put the power to prevent HIV in the hands of women.
We need
tools that will allow women to protect themselves. This is true whether
the woman is a faithful married mother of small children — or a sex worker
trying to scrape out a living in a slum. No matter where she lives, who
she is, or what she does — a woman should never need her partner’s
permission to save her own life.
Let me be
clear: As we discover and distribute preventive tools that women can use
without a man’s cooperation, we are not excusing men from their
obligations to be sexually responsible and to protect their partners. We
are just reducing the consequences to women if they don’t.
In a
moment, Melinda is going to discuss the research underway in microbicides
and oral prevention drugs — products that women could use to protect
themselves from infection.
While
there is promising research to report, the world, in my view, has not done
nearly enough to discover these new tools — and I include our foundation
in that assessment. All of us who care about this issue should have
focused more attention on these tools, funded more research, and worked
harder to overcome the obstacles that make it difficult to run clinical
trials. Now we need to make up for lost time.
We
believe that microbicides and oral prevention drugs could be the next big
breakthrough in the fight against AIDS. We are determined to help medical
science discover these new drugs and get them to the people who need them.
Melinda?
Melinda Gates:
Thank
you. Like Bill, I’m very honored to be here. Compared with so many of you,
Bill and I are relative newcomers to this cause, and we’re deeply inspired
by those of you who long ago committed your lives to ending AIDS.
When it
comes to stopping this disease, there is no silver bullet. We need to be
much more aggressive about getting all of today’s prevention tools to
everyone who needs them. And we need a constant stream of new innovations
— especially those that put the power to prevent HIV in the hands of women.
Of course,
the most highly anticipated milestone on this path is a vaccine. It’s a
major focus of our foundation, and we’re intensifying our efforts in this
area. Last month, we announced a series of grants to help develop and
evaluate vaccine candidates. These grants support the priorities that were
identified by the Global HIV Vaccine Enterprise, an alliance of
researchers, funders, advocates, and private industry that is dedicated to
speeding up the development of a vaccine.
But
finding an HIV vaccine is a long-term project. That’s why we have to
accelerate research on other preventive tools that can be available sooner.
As Bill
said, we believe the most promising breakthrough that could be available
soon is an effective microbicide or oral prevention drug.
Microbicides are gels or creams that women can use to block infection.
They’re the first preventive tools that would be intended specifically for
women’s use. Sixteen candidate microbicides are now being clinically
evaluated. Of those 16, five are in major advanced studies.
Another promising approach is an oral prevention drug. The hope behind
this research, as you all know, is that the anti-retroviral drugs that are
now used for treatment might also be effective for prevention.
Antiretroviral drugs have already been proven to lower the risk of
infection for babies born to infected mothers. Some have been successful
in preventing HIV infection in animals.
Drug trials are planned or underway in Peru, Botswana,
Thailand, and the United States. These studies are promising, but we need
more trials of more candidates in more places — for both microbicides and
oral prevention drugs — if we’re going to stop the spread of HIV.
The discovery of effective microbicides or an oral prevention pill is a
very exciting prospect. Bill and I are making it an immediate priority for
our foundation. But no discovery can save lives unless we distribute it to
everyone who needs it, and the record so far suggests we’ve got a lot of
work ahead of us.
Today,
fewer than one in five of the people at greatest risk of HIV infection
have access to proven approaches like condoms, clean needles, education,
and testing. That’s a big reason why we have more than 4 million new
infections every year.
Why aren’t
we getting these life-saving tools to the people who need them?
There are
many reasons — financial, logistical, political, social. But there is one
reason I want to emphasize today, and that is stigma.
The
simple fact is that HIV is transmitted through activities that society
finds difficult to discuss — activities that are infused with stigma — and
that stigma has made AIDS much harder to fight..
The image
of stigma was burned into my mind during a visit Bill and I made last
December to an AIDS hospice in South India. The patients in the hospice
were separated by gender. The long narrow trailer of the male ward was
filled with families and flowers. Children came to spend precious last
minutes with their fathers.
Across a
courtyard, we saw a very different scene. The female ward was a lonely,
desolate place. There were no visitors — just women wasting away from
AIDS. Some of them had managed to get themselves to the hospice; others
had been abandoned there by a relative who no longer wanted anything to do
with them. There was no love, no warmth, no comfort. Just wives and
mothers, left alone to die.
Stigma is
cruel. It is also irrational.
Stigma
makes it easier for political leaders to stand in the way of saving lives.
In some countries with widespread AIDS epidemics, leaders have declared
the distribution of condoms immoral, ineffective, or both. Some have
argued that condoms do not protect against HIV, but in fact help spread
it.
This is a
serious obstacle to ending AIDS. In the fight against AIDS, condoms save
lives. If you oppose the distribution of condoms, something is more
important to you than saving lives.
Some
people believe that condoms encourage sexual activity, so they want to
make them less available. But withholding condoms does not mean fewer
people have sex; it means fewer people have safe sex, and more people die.
When Bill
and I visit other countries, we are enthusiastically accompanied by
government officials on all our stops... until we go meet with sex workers.
At that point, it can become too politically difficult to stay with us,
and sometimes our official hosts leave.
That is
senseless. People involved in sex work are crucial allies in the fight to
end AIDS. We should be reaching out to them, enlisting them in our efforts,
helping them protect themselves from infection, and keeping them from
passing the virus along to others.
If
politicians need a more sympathetic image to make the point, they should
think about saving the life of a faithful mother of four children whose
husband visits sex workers. If a sex worker insists that her clients use
condoms, that sex worker is helping to save the life of the mother of
those children.
If you’re
turning your back on sex workers, you’re turning your back on the faithful
mother of four.
Let’s not
turn our back on anyone. Let’s agree that every life has equal worth and
saving lives is the highest ethical act. If we accept this, then science
and evidence — untainted by stigma — can guide us in saving the greatest
number of lives.
This is
the only way we will get the full life-saving power of the preventive
tools we have today and the ones we’re going to discover tomorrow.
If we’re
going to make dramatic advances in prevention, no one can go it alone. We
all have a role to play.
We at the
Gates Foundation will keep investing in research on microbicides and other
preventive tools. We will also do everything we can to remove the
roadblocks that stand in the way of trials.
I hope
AIDS activists will use their influence to push for more research into
prevention and to insist that we bring the tools we already have to the
people who need them. Nobody has the power you have to focus attention,
apply pressure, and get action.
You
proved this when you pushed for new treatment; the world now needs you to
push just as hard for prevention.
Governments should make the search for new prevention tools, such as
microbicides, a bigger priority in their budgets. If they can, they should
host clinical trials, and use their influence to help the trials run
smoothly.
Pharmaceutical companies can make a powerful contribution by spending more
on research and development for preventive tools, including microbicides.
But there is another exciting way in which they can contribute. Drug
companies have developed medicines to treat people with HIV. They should
do more to share these drugs with researchers who want to test whether
they can also be effective for prevention.
Researchers can help test the drugs more quickly by developing novel trial
designs, finding faster ways to analyze data, and coming up with
biomarkers that can help test a hypothesis without needing a clinical
trial of 10,000 patients. They should also make sure that when clinical
trials are run, they benefit those who are in greatest need.
The WHO,
UNAIDS, and other organizations should help develop common ethical
standards for clinical trials so they can start faster and run without
interruption.
If all
these players do their part, we will move forward, as fast as science can
take us, to discoveries that can help block the transmission of HIV. This
goal is worth our greatest efforts; it could very well be the turning
point that leads to the end of this disease.
In
closing, I want to say how deeply inspired Bill and I are to see so many
people gathered together here committed to this great cause. It is hard to
overstate the historic scale of our goal. In the history of human
accomplishment, ending AIDS will fill a category all its own. It will
stand as a work of scientific genius. It will be a testament to diplomatic
brilliance. It will represent enormous generosity of spirit and compassion.
But above
all — and unlike so many other great works — ending AIDS will not be the
success of one great scientist, one great community worker, or one great
leader; it will be an accomplishment of the whole human family working
together for one another. Thank you, once again, for dedicating your lives
to ending AIDS. We’re so honored to be part of your work.
Thank you.
Grandmothers going global - Aug. 14,
2006
The
Grandmothers to Grandmothers gathering has all the markings of
becoming a truly international movement.
Stars
such as U.S. Grammy winner Alicia Keys and actress Olympia Dukakis,
along with British pop singer Elton John, are throwing their weight
behind the cause of African grandmothers who have lost their children
to HIV/AIDS and now raise orphaned grandchildren.
As
ceremonies ended yesterday for the three-day grandmothers' gathering
in Toronto, the African grandmothers continued their joyous expression
of love and faith, singing, chanting and dancing.
But,
for UN Special Envoy for HIV/AIDS Stephen Lewis, it's just the
beginning. Lewis told the Toronto Star that the Stephen
Lewis Foundation has begun discussions with Keys and John to make the
movement a truly international one. Both stars have their own
charities involving HIV/AIDS and have expressed interest in helping to
get grandmothers from around the world involved.
"There
is a kernel here of something much bigger than itself," said Lewis
after the closing of the conference. "It seems we have the means of
lifting it off the ground and making it an international cause
célèbre."
Lewis's daughter, Ilana Landsberg-Lewis, who runs his foundation, came
up with the idea of bringing the grandmothers together. The Lewis
foundation funds HIV/AIDS programs in Africa.
Canadian grandmothers were asked to raise money to help their African
counterparts. What was to be a modest gathering of the Canadian and
African grandmothers just before the International AIDS Conference
took off and culminated with their message being beamed around the
world.
International news media — including CNN, the South African
Broadcasting Corporation and the BBC — jockeyed for space with local
media covering the closing session and a walk through Toronto's
downtown.
Early
yesterday morning the 300 grandmothers, bearing banners and signs that
called for an end to HIV/AIDS, were joined by singer Keys as they
marched and sang until they arrived in the atrium of the CBC Broadcast
Centre on Front St. Then Keys, hand in hand with Lewis and with an arm
wrapped around a Kenyan grandmother, ushered the women inside.
"I'm
honoured to be here marching with you," she said. "I feel like the
silence has been broken."
Keys
told the crowd she loves her own grandmother deeply and can't imagine
her losing her children and having to raise grandchildren. Keys didn't
perform but did join the grandmothers in a rendition of We Shall
Overcome. A videotaped message from Elton John was also played.
The
grandmothers presented a statement to Dr. Mark Wainberg, co-chair of
the International AIDS Conference, calling for more food, housing,
clothing and education for the African grandchildren. They also asked
for education and training for African grandmothers who feel
ill-equipped to raise children who are bereaved, impoverished,
confused and vulnerable.
The
recommendations also called for global action — including a pledge by
Canadian grandmothers to not only mobilize funds but also "apply
pressure on governments, on religious leaders and on the international
community."
"We
grandmothers deserve hope," Joyce Gichuna, a Kenyan grandmother, told
the crowd. "Our children, like all children, deserve a future. We will
not raise children for the grave."
Wainberg used the opportunity to deliver a scathing attack on Prime
Minister Stephen Harper. The Prime Minister has chosen not to attend
the AIDS Conference.
"I
don't understand why Mr. Harper fails to understand that HIV is the
world's public enemy No. 1 ... And why, given that HIV is the most
important enemy on this planet, is Prime Minister Harper not here to
show leadership on the world stage? As a Canadian it breaks my heart."
The
same can't be said for grandmothers attending the conference. Their
hearts were soaring as they headed home with a renewed sense of hope.
"I'm sure the world will now recognize the plight old people have been
through because of the pandemic," said South African grandmother
Princess Ntombenhle Mkhize.
"They
want the same thing we want for our grandchildren — a brighter
future," added Canadian grandmother Gisele Lalonde Mansfield, who lost
her brother to AIDS and is climbing Kilimanjaro next year in his
honour.
Clinton,
Gates urge more AIDS testing - Aug. 14, 2006
The
urgent need to stem the tide of new HIV infections is being undermined
by the fact too few people know their HIV status and are unwittingly
spreading the disease, former U.S. President Bill Clinton warned today
as he took the stage with Microsoft founder Bill Gates at the
International AIDS Conference.
“I
don’t see how we’re ever going to catch up, unless people are at least
aware that they could be giving the virus to other people,” Clinton
told a huge audience, drawn by the chance to listen to two of the
world’s most influential men — both committed warriors in the fight
against HIV/AIDS — expound on the issue in a panel jokingly referred
to as the double-Bill.
“We’re still behind the eight ball. And I think we’ve got to continue
to fight stigma and got to stop people . . . from being afraid of
being tested.”
Ninety per cent of HIV-infected people in developing countries don’t
know they carry the virus, Clinton noted.
In
many settings, people known to be HIV-positive are still ostracized.
And in places where there is no or limited access to life-saving
antiretroviral drugs, there may be little incentive to finding out
whether one is infected with the virus that causes AIDS.
The
scale up of programs to deliver badly needed AIDS drugs to developing
countries could start to chip away at that problem, Gates noted,
adding that having treatment broadly available “does start to change
the dialogue.”
But
cracking the nut of stigma will be difficult, suggested Gates, who
noted that in his travels to afflicted countries around the globe,
having a discussion with officials about the behaviours that fuel the
spread of the virus — unprotected sex and injection drug use — is
invariably an awkward encounter.
“I
haven’t come to a country where injecting drug use is easily discussed
or men having sex with men or commercial sex workers,” Gates said to
laughter and applause.
“I
hope to go to that country some day, where none of those things are
controversial or hard to discuss. But we don’t really have that.”
The
fight against AIDS has always been complicated by the way the virus is
spread, with moral and religious beliefs colouring responses on some
fronts. While public health experts cite sound evidence that needle
exchange programs and condom distribution save lives, some — including
the current U.S. administration — prefer to stress abstinence and
monogamy.
While
neither man overtly criticized that approach, they did suggest
over-emphasizing abstinence was ignoring the reality of human
behaviours.
“An
abstinence-only program is going to fail. And in the end you’re going
to wind up being in a cruel fix,” said Clinton.
The
session began with a minor demonstration, with a number of members of
the audience drowning out the moderator to demand affluent countries
stop poaching health-care workers from developing countries, a
practice that has left some of the world’s poorest countries bereft of
doctors and nurses.
“We
need more nurses,” the protesters chanted.
“I
actually agree with that,” Clinton said, taking the wind out of the
disruption. “We do need a lot more nurses.”
The
former president did not agree, however, to a request from the crowd
that he consider becoming Canada’s prime minister — a dig from an
audience member, perhaps, at Prime Minister Stephen Harper, who has
refused to attend the conference.
Clinton side-stepped the potentially awkward moment by
noting that he has been in Canada so often since ending his presidency
that he should check with his accountant to see if he ought to pay
Canadian taxes.
New HIV drug appears to be 'very
potent'
TORONTO
-- Patients taking a brand new type of HIV drug have shown a quick reduction
in the number of viruses circulating in their bloodstream, according to
early data from a clinical trial that is to be announced at the
International AIDS Conference in Toronto later this week.
The drug
belongs to a long-awaited new class of HIV medications known as integrase
inhibitors. They work to block the enzyme the virus uses to integrate its
genetic material into the DNA of a host's cell and make copies of itself.
As more and
more patients develop drug resistance to standard therapies, integrase
inhibitors are raising hopes of a new first-line treatment against the AIDS
virus.
"For people
with resistance to many different drugs, this [early study data] offers them
hope," said Martin Markowitz, one of the trial's investigators and a
clinical director at the Aaron Diamond AIDS Research Center in New York.
But Dr.
Markowitz, who is also a professor at Rockefeller University, cautioned that
"it is too early to predict where this will lead."
Merck & Co.
is developing the drug, one of two in the new class. Its compound, known for
now as MK-0518, is involved in an ongoing clinical trial with 198 HIV
patients who had previously been untreated for their infection. The studies
are being conducted at 28 different centres around the world, including two
in Canada.
At the
outset, the patients had to have at least 5,000 copies of the virus in every
millilitre of blood. They also had relatively low counts of the immune
system's CD4 cells, which HIV attacks. Cell counts averaged between 271 and
314 per microlitre.
(Treatment
usually begins when a patient has more than 100,000 copies of the virus or
below 350 CD4 cells). Most of the patients in the trial, 160, were given the
new oral drug in combination with two other antiretroviral therapies.
Thirty-eight were given an existing type of HIV medication as well as the
two other antiretroviral agents.
Based on
data at six months into the two-year trial, Merck reports that 85 to 95 per
cent of patients taking the integrase inhibitor drug regimen have seen their
viral loads plummet to less than 50 copies.
Patients'
immune-cell counts, meanwhile, increased by 139 to 175. Ninety-two per cent
of patients taking the older drug combination showed similar results, but
the effect took longer to achieve.
"What is
striking is the rapidity with which the patients reached these lower levels
[of viral load]," Dr. Markowitz said. "This looks to be a very potent drug."
The drug's
antiviral effect was seen in patients taking the oral drug at doses ranging
from 100 milligrams to 600 milligrams twice a day.
A press
release from Merck states that side effects in the trial have so far been "mild
to moderate, with nausea, dizziness and headache reported most frequently."
Dr.
Markowitz noted that 10 patients have discontinued taking the medication,
two for lack of efficacy, seven for reasons not related to the trial and one
because of an adverse effect related to liver function.
Mark
Wainberg, director of the McGill University AIDS Center and co-host of the
Toronto conference, said the results sound encouraging.
What's
more, Dr. Wainberg stressed, the research field desperately needs good news:
"It's pretty urgent. People are still dying of AIDS because they are
resistant to everything we have to treat them."
Researchers
have found integrase inhibitors difficult to develop in part because it
requires altering the viral genome without harming the DNA of the host. Dr.
Markowitz said it is satisfying to finally see the new drug class move into
clinical trials.
"We have
drugs that target two of three enzymes that HIV requires for its life cycle,"
he said. "This is like the third leg of the stool."
Tiny grants, big hope in AIDS
fight
In the
Mashuru area of Kenya, a single woman with HIV who had no source of income
now runs a small general store, is self-sufficient and, most importantly, is
eating properly, thanks to a $140 grant from World Vision.
In the same
region, a group of 15 women have used a $1,400 grant from the humanitarian
organization to expand a small business of rearing goats for sale at market,
using the added profit to care for HIV orphans and vulnerable children in
their village.
“What's
really crucial is to empower women to have a say in their lives so they can
become less vulnerable,” said Carole Leacock, a HIV/AIDS program specialist
with World Vision Canada, who noted that women in rural villages tend to be
more stable, while men often travel to get work.
Unlike big
business grants, injections of small amounts of money in Third World
countries can play a critical role in developing a thriving local economy.
That's
especially true in areas where disease has devastated households, creating a
situation that perpetuates poverty and undermines the community safety net
with people unable to care for themselves.
Ms. Leacock
gave an audience at the International AIDS Conference in Toronto yesterday
the results of a microfinance project in Mashuru, located about 120
kilometres southeast of Nairobi, where droughts in recent years have made
people living with HIV and AIDS destitute.
Forty-seven
microfinance projects last year gave people living with HIV and AIDS basic
business training that improved their disposable income, health, nutrition,
dignity and self-respect, as well as better access to anti-retroviral drugs,
and decreased the stigma of the disease, she said.
“No one is
going to bed hungry they were able to repair their houses, pay rents, create
assets and send their children to school. Today, they continue to be engaged
in gainful employment as small trades by reinvesting their savings.”
Ms. Leacock
also said people can now afford the $3 bus trip for a 50-kilometre monthly
visit to the nearest health facility that dispenses free anti-retroviral
drugs.
“Every time
we make a difference in one parent's life, we prevent another child from
become orphaned. And that's very important to us.”
Results of
another World Vision microfinance project in Tegucigalpa, Honduras, will be
released at the conference tomorrow.
Dina
Eguigure, a national manager of HIV/AIDS programs in Honduras, said that
results of a two-year project found that helping people with the disease set
up their own businesses increased “social inclusion of a group normally
excluded from the formal economy.”
Nearly
$50,000 (U.S.) was earmarked to help 150 families living with HIV, with 37
per cent of the money used by women with no formal education. Most women set
up small businesses attached to their homes, selling traditional foods,
small goods and second-hand clothes purchased elsewhere, she said.
“By the end
of the project, they paid up their credits with no outstanding debts,
showing their business skills and the solid coaching provided by the project
team.”
Largely
designed to improve the quality of life for adolescent women between 15 and
19 years of age and mothers living with HIV and AIDS, the project also
trained teachers and youth leaders about sexual and reproductive health, HIV
prevention and proper use of anti-retroviral treatments. It also
strengthened community grassroots organizations and helped develop stronger
government links, she said.

A place for medical marijuana
Nestled
in a corner of the AIDS conference's Global Village is a group of
individuals trying to raise awareness about the therapeutic benefits of
using cannabis to treat AIDS symptoms.
"It's a
serious crime that this plant is illegal in most countries," said Hilary
Black, a spokeswoman for the Medical Marijuana Information Resource
Centre.
In
Canada, which is the only other country aside from the Netherlands that
hands out licences authorizing the possession of medical marijuana to
people living with HIV-AIDS, only a quarter of those infected are
smoking the drug legally.
"The
information really needs to be out there because cannabis is saving
lives," Ms. Black said, adding that there is clinical evidence showing
that smoking it can alleviate nausea, increase appetite, and increase
adherence to HIV-AIDS medication.
This is
the first time medical marijuana has been represented at the
International AIDS Conference and the information booth has been a hit,
Ms. Black said.
"It's
actually being talked about professionally, rather than being giggled
about or talked about in the closet."
Hitting
the road for the cause
Princess Kasune Zulu's radiant smile and big eyes hide well the pain and
suffering she has seen in her 30 years.
After
losing her baby sister, older brother and both her parents to AIDS as a
teenager, the young Zambian couldn't deal with the pressures of heading
a household full of siblings and cousins looking to her as their only
hope.
She
dropped out of school and had a baby girl by 18, married her boyfriend
25 years her senior and had a second daughter right before they divorced.
But the
real blow came when she tested positive for HIV at 21.
"I was
not traumatized but rather filled with overwhelming peace," she said
yesterday. "My diagnosis was a spiritual awakening."
She
decided to hit the road with her status, against the wishes of the
church and her ex-husband. She dressed up as a "commissioned sex worker,"
walked along the highways of Zambia and hitchhiked with truck drivers.
Her intent was to tell them about the spread of HIV and her own
diagnosis because truck drivers were known to sleep with dozens of young
sex workers and be a conduit for infection.
"I knew
I had to reach the adult men and tell them what they were doing because
those young girls, you can't just tell them to stop. Those girls [were]
doing it to raise school fees, or buy their younger brothers and sisters
shoes to wear to school, sneaking out at night while their grandmother
is asleep."
Ms.
Zulu's story has been heard by presidents and heads of state around the
world. She is currently working on her book, I Will Not Die Before I'm
Dead: A Memoir of Hope in the World of AIDS, which will be released
next year
Four-drug cocktail no better,
study finds
TORONTO
-- Adding a fourth drug to the current triple-drug cocktail is no better at
treating newly diagnosed patients with HIV, according to a study released at
the International AIDS Conference yesterday.
The study,
published in the Aug. 16 issue of the Journal of the American Medical
Association, found that adding a fourth HIV drug, in this case abacavir, did
not reduce the amount of virus in patients' blood. Previous smaller studies
had been contradictory on the matter; some suggested that adding a fourth
drug could more quickly beat back the virus, while other studies did not.
This study,
which followed 765 patients over three years, found that in roughly 80 per
cent of the subjects, the human immunodeficiency virus remained suppressed
whether they were on the three- or four-drug cocktail, according to the
results released by Roy Gulick, director of the Cornell University HIV
clinical trials unit and associate professor of medicine at Weill Medical
College of Cornell in New York.
"It doesn't
look like adding a fourth drug to the very successful three-drug regimen
taken today provides any additional benefit," he said at a morning news
conference.
In the
study, 765 HIV-infected patients who had never received treatment were
randomly assigned to one of two regimens: a four-drug cocktail that included
zidovudine, lamivudine, abacavir and the non-nucleoside drug efavirenz; or a
three-drug cocktail of zidovudine, lamivudine and efavirenz.
According
to Dr. Gulick, the rationale for the study was predicated on past success:
Since the triple-drug cocktail worked better on HIV patients than the
two-drug cocktail, researchers wanted to learn whether four drugs would be
better.
In the
study, which ran from 2001 to 2005, roughly the same number of patients in
each group (88 per cent in the four-drug group and 85 per cent in the
three-drug group) achieved undetectable levels of virus in their blood.
After three years, 25 per cent of the four-drug group and 26 per cent of the
three-drug group achieved so-called virologic failure, which meant that the
drugs were no longer effective at reducing the levels of virus in their
blood, according to the study, which was supported by grants from the U.S.
National Institutes of Health.
The Aug. 16
JAMA issue was published to coincide with the AIDS conference; its contents
are devoted entirely to HIV/AIDS. Another study in the issue found that
rapid expansion of free anti-retroviral therapy programs in Zambia produced
favourable outcomes.
At the news
conference yesterday, JAMA editor-in-chief Catherine DeAngelis said the AIDS
epidemic now matches the deaths from the bubonic plague.
About 25
million people have died of HIV/AIDS in 25 years and about 40 million people
currently have it. Anti-retroviral medications have turned HIV/AIDS, once a
death sentence, into what many consider a chronic disease.
Simple solutions to save
newborns
There was
lots of buzz, at the opening of the 16th International AIDS Conference
yesterday, about the new: new drugs; new technologies; new deals on funding
and drug access.
Far away
from the buzz, clinicians from the developing world talked about keeping
pregnant women from passing the AIDS virus on to their babies.
There is
nothing new about this: We've known how to do it for nearly a decade. It's
cheap, and it's one surefire way of cutting down on new infections. And?
More than 90 per cent of pregnant women with HIV around the world do not
have access to any of the simple interventions that would keep them from
infecting their babies. Seventy children an hour are infected with the virus
by their mothers, and 45 die every hour from AIDS.
These
numbers suggest that in all the understandable hunger for the new in AIDS,
we have lost sight of the fact that we haven't yet figured out how to solve
one of the most basic problems. And because this is a problem of women --
poor, rural women in Africa, in particular -- it has slid quietly to the
bottom of the international AIDS agenda.
Women
infect their babies with HIV three ways: roughly a third of them in utero; a
third in delivery; and a third through breastfeeding.
Fewer than
500 children will be infected in North America this year, because it's very
easy to prevent all three. If a woman doesn't breastfeed, if she delivers by
cesarean and if she and her baby are given an anti-retroviral drug before or
during labour, the risk of transmission is less than 2 per cent.
Of course,
not every rural health clinic in Rwanda can provide a cesarean section. And
not every Rwandan woman can feed her baby with formula safely, because many
lack clean water. But the drug intervention -- that's easy. A single dose of
the drug nevirapine can cut transmission by at least 30 per cent. That costs,
at most, a couple of dollars, and manufacturer Boehringer Ingelheim donates
it free in many parts of the world. Using two or three ARV drugs together
can lower transmission by much more. But less than 9 per cent of pregnant
women worldwide get any of these interventions.
African and
Indian doctors talked about how they lack the labs and the staff to test and
counsel all the pregnant women; how the women they see may come for an HIV
test but never return for drugs because they live too far away and can't
afford to take another day off work to wait in line at a busy clinic.
Dr. Agnes
Binagwaho, who heads the national AIDS agency of Rwanda, talked about her
country's program, which is, by African standards, a remarkable success:
They're reaching 22 per cent of HIV-positive pregnant women with single-dose
nevirapine. But that program is now imperilled. "We had funding from the
Global Fund," she said, money they used to build labs and train and pay
staff. "But that funding ends now."
Arletty
Pinel, of the UN Population Fund, says the fact that more women don't get
this service reflects the overall low priority put on maternal and
reproductive health. These programs are almost universally minimally funded
and minimally staffed, she said, and so it's no surprise that more women
with HIV don't get the basic interventions. "Getting a pregnant women who is
HIV positive is remedial, it's damage control -- and we don't do damage
control well."
The World
Health Organization announced yesterday that it now recommends putting
pregnant women with AIDS on full ARV therapy from 28 weeks of pregnancy. A
fine idea, but if less than 9 per cent of women are receiving a one-off drug
dose, how on earth are Rwandan clinics that just lost their funding going to
do full therapy?
One of the
big topics at the conference this week is pediatric AIDS. It's high time
that pediatrics got more attention. But in all those sessions yesterday, no
one mentioned that there would be no need for pediatric treatment, if we
just mastered the one-stop intervention that keeps mothers from infecting
their kids
Prevention tools for women
urged
Toronto
— Women's issues were front and centre Monday at the International AIDS
Conference as Melinda Gates called for prevention tools for women so they
don't become infected by HIV.
“The two
that are on the horizon that I think really could change the face of this
disease are a microbicide, which is an odourless clear gel that a woman
would use vaginally to block the disease, or an oral prevention drug that a
women could take every day without her partner knowing,” she told a panel
discussion entitled Women at the Frontline in the AIDS Response.
But money
isn't the only obstacle in bringing these products to market, and making
them accessible to women in developing countries who can't protect
themselves against infected partners who don't use condoms.
“It really
comes down to trials,” said Ms. Gates, who together with her husband
Microsoft chairman Bill Gates gave a keynote address to open the conference,
and recently announced $500 million (U.S.) in funding to the Global Fund to
Fight AIDS, Tuberculosis and Malaria.
“We have 16
microbicide candidates today that are in first-stage trials, we have five
that are on their way to second-stage trials, but the truth is we need an
even more powerful microbicide than what's in trial today,” Melinda Gates
said.
“And a lot
of trials, both in microbicides and an oral prevention drug — in some ways
what's even more promising — have been stopped. And so we need to have more
trial sites created. We need more communities involved. We need more people
willing to come forward to participate in trials.”
Activists
need to make sure trials are ethical and done according to best clinical
practice methods, she said. But they also need to insist that trials be done.
Musa (Queen)
Njoko, a jazz artist and HIV activist in her native South Africa, was also
on the panel. She was one of the first women and the first recording artist
to disclose her HIV-positive status in South Africa.
“We need no
longer continue having our lives controlled by other people,” she said.
“It's our time, it's our lives, let's fight for our survival, let us fight
for the future of our children.”
Earlier
Monday, more than a thousand people from around the world took part in a
march and rally near the conference site to demand urgent action for women
and girls in the HIV/AIDS pandemic.
“Violations
of women's and girls' human rights have a direct impact on HIV infection,”
Louise Binder, co-founder of the Blueprint for Action on Women and Girls and
HIV-AIDS, said in a statement.
“Violence
against women and girls, poverty, lack of education and housing, and lack of
property rights, all fuel HIV/AIDS infection rates among women and girls.
HIV positive women's human rights are also regularly violated.”
Worldwide,
almost 50 per cent of all HIV positive adults are women over 15 years old.
In Canada,
women represented 27 per cent of positive HIV tests in 2005.
Unique
tribe of activists stands ready to shame the negligent and the greedy
- Aug. 15, 2006
These
are some of the tools AIDS activists like Paul Davis use to fight the
lethal virus: fake blood and banners, padlocked lengths of chain, foam
sculptures — and this week, maybe even a few funeral urns.
It's
a far cry from the orthodox measures employed in the high-stakes
medical battle. While infectious-disease researchers, politicians and
aid agencies this week discuss advances in protease inhibitors or safe
needle exchange programs, Davis and about 1,000 other activists have
flocked to Toronto to protest allegedly greed-fuelled drug companies
and idle politicians.
With
22,000 delegates and 8,000 journalists, exhibitors, volunteers and
staff at the mammoth International AIDS Conference, there is no better
opportunity to spotlight their gripes.
"We're
trying to capture the imagination of the public and provoke a response
from decision-makers," said Davis, who has worked with the group Act
Up Philadelphia for 13 years.
For
the past few days, dozens of activists have been stationed at the
University of Toronto, formulating plans behind closed doors and
conducting informal sessions for nascent protestors on how to interact
with reporters.
Yesterday, activists held a small protest at the Metro Toronto
Convention Centre. But they pledge more to come.
At
past conferences, protestors have held mock trials for world leaders
and staged "die-ins," zipping themselves into body bags, or "chain-ins,"
chaining themselves to fixed objects.
"A
lot of what we do is street theatre," said Eric Sawyer, a New Yorker
who has helped launch three AIDS groups. "We basically won't do
anything that might cause physical harm or permanent damage, but
anything else goes — and embarrassment is a big tool."
When
it comes to humiliating political or corporate leaders, several
activists said Davis, 36, is as gifted as they come. One idea he said
he might try this week would be to buy funeral urns to "present" to
drug company officials.
"To
play off the `You earn, we urn' angle, you know?" Davis mused.
Matthew Kavanagh, of the Student Global AIDS Campaign, said one
prospective target this week is Abbott Laboratories, which has been
criticized for not providing broad access in Africa to a new version
of its Kaletra medication that needs no refrigeration.
Toronto Police Insp. Donald Campbell, who is overseeing policing at
the conference site, said no arrests had been made there as of early
last night, perhaps as a result of a meeting he held with activist
leaders last week.
"We
basically went over Canadian law, talking about what constitutes a
criminal act and what they are allowed to do," Campbell said. "We
talked about whether putting stickers on a company booth is criminal
and things like our release laws." It's possible that a non-Canadian
arrested in Toronto would have to post bond as high as $500 to be
released, Campbell said.
"I
think it's great that we were able to sit down in the same room
together," Campbell said of the meeting. "That wouldn't have happened
10 years ago."
Hokey
or not, activists have proved deft at grabbing attention since the
inaugural AIDS conference in Atlanta in 1985. They've stoked
controversy by crumbling a communion wafer at St. Patrick's Cathedral
in New York; halted trading at the New York Stock Exchange; decorated
a float at New York's Gay Pride parade as a concentration camp; draped
a huge condom over the home of U.S. Senator Jesse Helms; and dumped
the ashes of AIDS victims on the White House lawn.
At
the Barcelona AIDS conference in 2002, activists stormed the stage,
interrupting a speech by U.S. Secretary of Health and Human Services
Tommy Thompson. Screaming "Shame!" they bore signs that accused the
U.S. of murder and neglect because it hadn't committed enough to AIDS
research and prevention. When they were forced offstage, whistles and
jeers drowned out the rest of Thompson's speech.
Two
years ago, at the Bangkok conference, it was a new drug trial in
Cambodia that raised activists' hackles. They charged that sex workers
and other marginalized people had been recruited for the trial because
they didn't have the leverage to negotiate insurance or a pledge that
they would be cared for if they fell ill during the trial period.
Act
Up Paris and some prostitutes stormed a stage during a scientific
session and splattered company booths with fake blood. "I don't know
what they use, but it's the perfect consistency of real blood," Davis
said, enviously. "It's some sugary concoction."
Not
every protest goes off as planned.
At
the Toronto opening, some protestors held aloft lab coats
spray-painted with slogans to highlight a lack of health care workers
in Africa.
Waiting beside the stage for his turn to speak, Microsoft's Bill Gates
squinted at the offerings before turning to his wife and asking: "What's
it say? They should have made the words bigger."
Nevertheless, AIDS activists contend their actions have helped to
speed up clinical trials and lower their cost.
"We
basically said, `Look, our people are dying right now and are going to
be dead by the time the government makes sure a new drug was safe,'"
Sawyer said. "We had nothing to lose by taking it sooner."
Orphan' virus could help fight
HIV
A benign virus that can
float harmlessly in the human bloodstream for years may be able to
reduce transmission rates of HIV from mothers to their infants
seven-fold, a University of Toronto study suggests.
The
virus, a close relative to potentially lethal hepatitis pathogens, has
also been shown to inhibit the ability of HIV to infect its target
blood cells, U of T researcher Wendy Supapol said yesterday during a
presentation at the 16th International AIDS Conference.
Researchers say the virus — known as GBV-C — has the potential to form
the basis of an AIDS vaccine.
"That
would be the hope," said Dr. Peggy Millson, of the university's public
health sciences department. But much further study must be done first.
Millson said if GBV-C does prove to be as benign to humans as it
appears, "prevention strategies related to using this virus" might be
possible.
U of
T officials have billed the study as one of the most exciting of
several dozen research projects the university is presenting at the
conference.
In
the study, which followed 1,440 HIV-infected mothers in Thailand — 19
per cent of whom also carried active GBV-C — the rate at which HIV was
passed from infected mothers to infants plummeted when GBV-C was also
transmitted to the child during the pregnancy or at birth.
"If
the mother managed to transmit (GBV-C) to her infant, as happened in
about 41 per cent of cases ... their (babies') chance of being
HIV-infected was only 2 per cent," says Supapol, a PhD student in
epidemiology. "In the GBV-C negative infants, it was 13 per cent."
The
virus, discovered in 1996, bears a 98 per cent genetic resemblance to
hepatitis C. Unlike that liver-destroying virus, however, it appears
to have no harmful effect, Supapol says. "They call it an orphan
virus; it's not known to cause any disease in humans."
And
unlike other forms of hepatitis that can actually make HIV more lethal,
GBV-C has been shown in several studies to lessen the impact of the
AIDS-causing virus.
"This
is the only one of the co-infections that we know of that seems to be
beneficial," Millson said.
"So
understanding more about why this virus does not do those bad things
and why it may actually be beneficial to preventing transmission would
be really valuable."
Studies have shown that HIV-positive people who were also GBV-C
positive fared better than those who had HIV alone, Supapol said.
Several long-term studies showed that HIV-positive people who
maintained GBV-C in their system remained healthier than those who
lost the tame virus over time.
But
is it the virus itself that is blocking HIV transmission and damage —
or a related process that remains hidden? Researchers are split on
that question.
"One
group thinks GBV-C has beneficial effects ... the other ... that it's
probably due to something else," Supapol says.
But
Supapol says compelling laboratory studies have shown that the virus
is able to block HIV receptors on human T-cells, locking the
AIDS-causing pathogen out of its target host.
In
these test-tube experiments, GBV-C reduced the actual number of
receptor doorways on the cell surface. The studies also showed a 99
per cent reduction in HIV infection of white blood cells that were
previously exposed to GBV-C.
But
there's no evidence yet, Supapol says, that GBV-C by itself can
protect against HIV infection in adult humans.
We need to take the lead'
In India, many
HIV-positive women are stoned to death so their families don't have to
live with the shame.
These women are
trapped in the cultural norms of their homeland; they grow up to be
dutiful and agree to arranged marriages and become dutiful wives, Dr.
Nafis Sadik, United Nations Special Envoy for HIV/AIDS in Asia, told a
symposium yesterday.
The women know
nothing about AIDS or their own sexuality and it's only when they
become pregnant they find out they have HIV, Sadik said. Then their
families blame them for bringing this horrible disease upon them; in
many cases, the HIV-infected women are killed.
Sadik said these
women are getting infected by their spouses and are then being
punished.
"It makes my blood
boil ..." she said. "Gender inequality is now one of the principal
drivers of HIV infection."
It's time for women
in developing countries to have more sexual equality if they want to
combat the virus, she said, adding that, in India, only 8 per cent of
women know anything about HIV/AIDS.
If current trends
continue, more women than men will be infected with HIV/AIDS.
With that statistic
in mind, a panel of women speakers told a symposium at the
International AIDS Conference that it's time for women to take
control.
"It's time to empower
women," pleaded Musa Njoko, 33, a South African jazz artist and HIV
activist who found out she had the virus when she was 22. "We need to
take the lead as women to take charge of our own situation."
Zambia suffering doctor
shortage
A doctor shortage in
Zambia — one of the countries hardest hit by AIDS — is so severe that
non-doctors are being used to help hand out free medication to the
nearly 30,000 patients in need of lifesaving drug therapy.
"It's a disaster,
it's the only way to describe it," said Dr. Moses Sinkala, director of
health in Lusaka District, Zambia, one of the poorest African nations.
There is no choice
but to have medication handed out by nurses and other health
clinicians because of the enormous "brain drain" of health care human
resources Zambia faces, said Dr. Jeffrey Stringer of the Centre for
Infectious Disease Research in Zambia, and of the University of
Alabama.
The U.S. government,
the Global Fund and the Zambian government have provided about $600
million to Zambia's AIDS fight since 2002.
The treatment
program's funding is secure until 2008. If it isn't continued, the
result will be genocide, Sinkala said yesterday after a news
conference at AIDS 2006, the 16th international AIDS conference.
Close to 22 per cent
of adults living in Lusaka, Zambia's capital, have the human
immunodeficiency virus (HIV). Last year, in the nation of 11.5 million
people, 98,000 Zambians died of acquired immunodeficiency syndrome
(AIDS).
The huge scale-up of
HIV/AIDS treatment programs in city centres in Zambia — making it the
largest single group of anti-retroviral patients being studied in this
part of Africa — is making a difference, Stringer said during a news
conference hosted by the Journal of the American Medical
Association. "The majority of patients we saw, if they didn't
start treatment, they would've died."
In 2002, the Zambian
ministry of health began distributing anti-retroviral medications at
two of the country's largest hospitals.
The program filled up
quickly and in 2004 it was expanded to clinics in the Lusaka urban
district.
New AIDS pill gets key
approval
A new
generic AIDS drug developed by a Toronto company jumped another hurdle
yesterday in its circuitous route to Africa when the World Health
Organization gave it a stamp of approval.
It's
a critical step if Apotex Inc.'s generic Apo-triAvir is ever to reach
patients in developing countries where HIV/AIDS is rampant. The WHO
endorsement is important because many African states don't have their
own drug regulators and trust the judgment of the international agency.
But
there are still troublesome obstacles to getting the new drug to
Africa and elsewhere, not the least of which is faulty federal
legislation.
The
legislation, called Canada's Access to Medicines Regime, was
originally intended to help Third World countries get cheaper generic
drugs to treat AIDS, malaria and tuberculosis.
The
bill stipulates that talks between a drug's patent holder and a
generic company hoping to reproduce the drug, should last at least 30
days before the generic firm can go to Health Canada and ask for a
compulsory licence. This would then allow the generic to bring its
cheaper version of a drug to the market.
But
the legislation sets no time limit on how long talks can last, which
is causing a deadlock.
If
the generic firms don't get approval from the patent holder, they
could be sued for patent infringement. So it behooves any generic
manufacturer to get brand-name manufacturers on side.
Apotex president Jack Kay said if the Canadian government wanted to,
it could change the regulations affecting the act.
"They
could do it tomorrow if they want," Kay said. "They'd probably say
they need to do a regulatory input analysis first, but that's just
politics."
Kay
said if Health Canada was going to approve a so-called compulsory
licence for the Apotex drug, the company could begin making batches
and be ready to ship it overseas within weeks.
A
Health Canada spokesman did not respond to emails and couldn't be
reached on the phone last night.
Negotiations with the patent holder, in this case GlaxoSmithKline,
have dragged.
Kay
said he has been continually snubbed in attempts to talk with
GlaxoSmithKline, which holds the patent on nevarapine. "I called (Glaxo
president) Paul Lucas more than five months ago and he just said, `I
can't deal with you, you have to talk to the lawyers,'" Kay said. "They're
only doing this to gum up the works."
The
lawyers for GlaxoSmithKline have insisted that Apotex show that the
large white tablets it will distribute in Africa don't resemble
comparable drugs in Canada, Kay said. Trouble is, Glaxo doesn't sell
the same medicine in first world countries because antiretrovirals are
more effective.
A
GlaxoSmithKline spokesperson didn't return a call for comment.
AIDS
experts are excited about Apotex's Apo-triAvir because it contains
nevarapine instead of Stocrin, also known as D4T, which cannot be
taken by pregnant women because of its side effects. Nevarapine also
has the added bonus of helping to prevent babies from contracting AIDS
from their mothers.
Apotex started working on the medication, which combines three drugs
in a single pill, in May 2005. It was submitted to Health Canada for
approval in December and was granted approval in July.
Doctors Without Borders has agreed to pay 38 cents per pill for the
Apotex drug, which won't cover Apotex's $2 million-plus worth of
research and legal expenses so far, Kay said.
Since
the federal legislation was passed two years ago, not one pill of any
generic drug has made it to Africa or any other developing nation.
Doctors Without Borders has been a fiery critic of the process. Rachel
Kiddell-Monroe, head of the humanitarian group's Campaign for Access
to Essential Medicines, is scheduled to speak at the International
AIDS Conference in Toronto, where she will call on Ottawa to
streamline the legislation.
She
also will urge other countries to bypass patent laws to get
antiretrovirals and other drugs to sick and dying patients.
The
just-announced WHO approval for the Apotex drug is important because
some African states don't trust other regulatory agencies. For
instance, in 2004, when the U.S. Food and Drug Administration approved
nine generic AIDS medicines for export, countries such as Nigeria,
Kenya, Ethiopia and Uganda wouldn't allow them into the country.
"Once
a drug is approved by the WHO, it can be bought by developing
countries who need it safe in the knowledge that it is effective and
safe for their people," said Kiddell-Monroe. "... Since there are so
many different drugs around, many of which are of extremely doubtful
quality, (developing countries) need somewhere they can look and be
sure drugs are appropriate."
Actor Gere cautions India about
American mistakes
TORONTO
— Actor Richard Gere brought his star power to the International Aids
Conference yesterday, calling HIV-AIDS the “true terrorist on the planet
today.”
At a news
conference to announce a public-service campaign in India, Mr. Gere said he
has been involved in the HIV-AIDS movement since the 1980s and hopes India
does not make the same mistakes the United States did in dealing with the
epidemic.
“It is
deeply important to me that India not make the mistakes we made in America,”
said a silver-haired Mr. Gere, looking relaxed in a blue shirt and tan suit
jacket. “We had no leadership. We didn't take it seriously and hundreds of
thousands of people died who didn't have to.”
A report
released last week by India's Registrar-General and Census Commissioner
estimated that about 11 million people in India could die of AIDS-related
illnesses by 2026. Based on demographic trends, the report said an
additional five million children who might not be born as a result of the
early deaths of HIV-positive women could be “missing.”
Yesterday,
Mr. Gere sounded hopeful about India, saying the incidence of HIV is
currently running at about 1 per cent of the population. If India is able to
keep it at that level, “there's a good possibility we are not going to see
10 million or 20 million more die,” he said.
At
yesterday's news conference, the Heroes Project, of which Mr. Gere is a
co-chair, and STAR India, the leading television network in India, announced
a two-year extension of their HIV-AIDS stigma reduction and prevention
campaign through the use of public-service television messages, many of
which send the message: “No Condoms, No Sex.”
As he has
grown older, the New-York-based movie star explained that he has had to make
some hard decisions about how he is to make his remaining years the most
meaningful he can.
“Probably
the most important [issue] to me was HIV-AIDS,” he said. “It's the true
terrorist on the planet today.”
Red tape stalls AIDS relief -
Aug. 16, 2006
Health Minister Tony Clement says he's launching an immediate review
of why Canada has failed to deliver on a pledge to get low-cost AIDS
drugs to countries in need.
He
has his work cut out.
There
are critical hurdles to be overcome, according to industry officials
and experts interviewed by the Star. They include: a lack of
financial incentives for generic drug companies; the cumbersome
process for acquiring licences to produce the drugs and, most
problematic, deep-rooted hostilities between generic and brand-name
drug companies.
"Exhibit
A is not a single pill has flowed through the system and got to the
people who need it," Clement said yesterday during a session on
vaccines at the International AIDS Conference in Toronto. "We need
legislation that works."
Everything is on the table, according to Clement, including forcing
brand-name companies to relinquish their patents through issuing
compulsory licences."It's all money," said Ariel Katz, a University of
Toronto professor who studies intellectual property and competition
law. "It may be good for generic companies to get involved in this if
they can win some points on the PR front, but if it's not going to
make any money, then why bother?"For most generic drug makers,
navigating the legislation isn't worth the effort.
Just
making pills for export to Africa is an unwieldy proposition. From
shape and colour to markings and packaging, tablets or capsules
produced for export can't in any way resemble those sold here by
brand-name drug makers."If you're going to make the pill blue if the
brand-name version here is white, you have to show that the new (blue)
coating still dissolves properly in the stomach and that the chemical
compound of the drug doesn't change," said David Windross, an
executive with generic drug maker Novopharm Ltd. "It just adds another
layer of research."
The
legislation currently caps the price at which generic drug makers sell
medicines to Africa at 25 per cent of what brand-name companies charge
in Canada.
At
least six generic drug makers have been briefed by Health Canada on
the act but only one — Apotex — has made any movement toward obtaining
a licence.
Under
the legislation, a company that wants to export a generic drug to
Africa, where an estimated 25 million people south of the Sahara are
believed to be infected with HIV, needs Health Canada approval even
though it will never be sold here. Next, a company must request a
voluntary licence from the drug's patent holder. If the patent holder
resists, the government can grant a compulsory licence.
But
AIDS activists say the legal wrangling has no limit. Most brand-name
drug companies and their generic rivals are often ensnared in legal
battles over more popular for-profit drugs; industry sources say it's
doubtful any companies would ever reach an accord on a so-called
voluntary licence — even if the medicines were sent to Africa.
"How
do they feel about us? They hate our guts," said Jack Kay, president
of Apotex, a Toronto-area generic pharmaceutical company that wants to
sell a new AIDS drug to Doctors Without Borders, an aid agency that
would then sell it or give it away in developing countries.
Apotex is at a stalemate with giant drug maker GlaxoSmithKline to
include the drug Zivudine in a new triple-pill antiretroviral that
could extend the life of AIDS patients for several years.
Correspondence between the companies, obtained by the Star,
suggests there's little willingness to bend on either side.
While
Kay said he first phoned Glaxo executive Paul Lucas in late 2005, it
wasn't until May 11 that an Apotex lawyer formally requested a
voluntary licence to make a generic version of three patented drugs
that would be included in the pill.
In a
June 9 letter to Apotex, Joy Morrow, a lawyer for Glaxo, replied that
Apotex had failed to indicate the specific country to which the drug
was to be exported.
Morrow also wrote that the request for a "royalty-free licence is not
reasonable. Our clients understand that ... Apotex is selling the
product at its own cost and requests a royalty-free licence," Morrow
wrote. "Our clients reserve their right to have such a statement
verified by independent auditors to verify the claim of non-profit
supply ... ."
Glaxo
said in a statement to the Star that "we are still waiting to
hear from them."
Kay
said Glaxo is resisting because, "it's the thin edge of the wedge.
They don't want to open any doors down the road to having exceptions
granted on their patents."
Glaxo
is one of the biggest pharmaceutical companies in the world and it
appears to have as much money invested in researching new drugs
against infectious disease as anyone.
Glaxo
is involved with 28 AIDS-related clinical trials, including eight that
are related to mother-to-child transmissions, said Dr. Lynn Marks, a
Glaxo senior vice-president and infectious disease researcher.
"As
far as I know, we're the only company out there that's trying to
develop a vaccine for AIDS, malaria and TB and is also working on
developing treatments for all of those," he said.
Glaxo
defends its requirement that Apotex produce unique colours and
markings for any drugs destined for Ghana, Zambia or other
impoverished countries.
"Otherwise,
the humanitarian spirit of this voluntary licence will be undermined
if the medicines produced for export do not reach their destination,"
Glaxo's statement read.
Several drug industry lawyers who specialize in patents said that for
generic companies, churning out low-cost drugs would mean halting
production on more lucrative product lines.
"Fact
is, generic companies don't have to invest in research and development
to bring a new drug to market, yet they still sell generic versions
for 70 per cent of what a brand-name drug costs," said one lawyer who
specializes in drug patent matters. "No one is doing this out of the
goodness of their heart."
Clement said the government intends "to do this comprehensively, do it
rationally to get some good information and advice because really this
is our first opportunity as a new government to consider this
legislation."
But
Stephen Lewis, the United Nations special envoy for HIV/AIDS in
Africa, was skeptical of when the review will be held.
"This
gives new meaning to the word immediate. They were elected eight
months ago. If this is the nature of their particular dictionary, I
wouldn't trust any word."
If
there was a sense of urgency about it, the review would already have
happened six months ago, he said.
"We've
lost another six months, in other words, and now we'll lose even more
time."
Clinton's recipe of hope - Aug. 16,
2006.
Bill
Clinton has a recipe to solve the world's problems: stop the devastation
created by AIDS.
"If we
could turn the tide of this epidemic, it will unleash a burst of energy
and belief in human potential that I think will spill over into
tuberculosis, malaria, economic development, climate change and anything
that we can possibly imagine," Clinton told the 16th International AIDS
Conference yesterday.
But the
former U.S. president, who turns 60 Saturday, admitted a vaccine is likely
a decade away.
He
emphasized universal treatment was the goal, but as long as millions of
people were becoming infected, it is difficult to attain. He said
prevention has to be as important as treatment.
Clinton
said male circumcision could slow down the spread of the disease, but
cautioned getting the world to accept this practice will be difficult.
"We will
have another job to do, a big job, first in selling it and secondly in
providing safe, effective, comprehensive and rapid ways of doing it," he
said.
Bill Gates to China: Will
$200M help?
The
Bill and Melinda Gates Foundation is close to reaching a landmark
agreement to start an AIDS initiative in China that's worth $200
million (U.S.), the Toronto Star has learned.
While
UNAIDS estimates 650,000 Chinese are said to be infected with HIV —
India and South Africa alone combine for more than 10 million cases —
infectious disease experts say conditions are perfect in China for the
disease to spread.
The
communist Chinese government for years denied the existence of AIDS
within its borders and many doctors have refused to diagnose it. The
government also tried to cover up an outbreak of HIV in central China
that was caused by a tainted blood-selling program.
But
more recently, President Hu Jintao has visited AIDS patients in
hospitals and has gone on the offence against infectious diseases.
The
Gates Foundation has become one of the world's most influential
philanthropies. Headed by Gates, the world's richest man, and his wife,
the foundation is the world's largest with assets of more than $30
billion.
This
summer, billionaire Warren Buffett pledged to give much of his fortune
to Gates's foundation, effectively doubling its spending power.
Carmine Bozzi, a Gates Foundation official who has led talks with the
Chinese government, confirmed yesterday that the foundation and the
Chinese are in final-stage talks to sign a memorandum of understanding.
"The
big problem in China is IV (intravenous) drug use," Bozzi said, adding
that the Gates program would largely be based in urban centres.
While
Bozzi declined to share specific details about the size of the Gates'
prospective investment in China, officials with other nongovernmental
organizations said it would total close to $200 million over five
years.
The
donation would be similar in size to the Gates Foundation's project in
India, where the group Avahan — which means "call to action" — is
promoting condom use, heightening awareness of high-risk sexual
behaviour and improving the diagnosis and treatment of sexually
transmitted infections.
China's infection rate is low, at about 0.1 per cent, but the virus is
spreading fast. Last year, there were 70,000 new HIV infections in
China, according to UN statistics.
"What's
scary about China is how quickly the disease could spread there," said
Joe Amon, head of the AIDS program with the aid agency Human Rights
Watch.
"If
you have 1 million people infected and perhaps another 25 million
people in high-risk situations — sex-trade workers, IV drug users and
gay men — and no education program, how fast could it spread?"
Amon
said the AIDS situation in China is comparable to some jurisdictions
in Russia, where, due to drug users sharing dirty needles, infection
rates have spiked to 50 per cent from 2 per cent in just two years.
Amon
said that while the Gates Foundation is dealing with China's health
ministry, ultimately the justice ministry will likely determine the
program's success.
"They
are going to control access to IV drug users and other high-risk
groups."
China
has also accepted a $95 million (U.S.) grant from the Global Fund to
Fight AIDS, Tuberculosis and Malaria to launch a drug program that
would provide free anti-retrovirals.
A
year ago it allowed the Clinton Foundation, organized by former U.S.
president Bill Clinton, to establish a toehold in the country.
Clinton's group signed a deal with Mchem Pharma Group of Xiamen to
provide low-cost chemical ingredients to companies that make generic
AIDS drugs in India and Africa.
US criticised for HIV aid
effort
Stephen
Lewis, UN Special Envoy on Aids, said President George Bush's $15bn
Emergency Plan for HIV/Aids was too focused on promoting abstinence.
He said
Washington was practising "incipient neo-colonialism" by telling African
nations how to fight Aids.
He also
accused the West of failing to deliver on funding commitments they had made
to fight the disease.
Speaking at
the 16th International Aids Conference in Toronto, Mr Lewis said: "No
government in the Western world has the right to dictate policy to African
governments around the way in which they respond to the pandemic."
Sub-Saharan
Africa remains the epicentre of the Aids pandemic, with two-thirds of all
people living with HIV coming from the region.
Two million
people died of Aids in the region last year and there were 2.7m new
infections.
The Bush
administration backs an "ABC" plan to fight Aids: Abstinence until marriage;
Being faithful to one sexual partner; and if those conditions are not
practised, the use of Condoms.
In 2003,
the US Government approved a $15bn package over five years to fight the
spread of Aids.
Abstinence
programmes
But the US
Congress has stipulated that a proportion of the funds must be spent on
encouraging abstinence-until-marriage programmes.
Mr Lewis
said abstinence programmes had been shown not to work.
"That kind
of insipient neo-colonialism is unacceptable.
"We're
saying to Africa: 'This is how you will respond to the pandemic' and that's
not appropriate because African governments are eminently capable of
deciding what their priorities are and what the response should be."
"You do not
provide money on the condition that they reflect your ideological priorities."
Top US
officials have rejected the criticism, denying it promotes abstinence to the
detriment of other HIV prevention strategies, or that it is designed to
appease conservative Republicans.
Mark Dybul,
US Global Aids coordinator, said only 7% of funding for 2005 had been spent
on abstinence programmes.
He said: "There
is no evidence in support of what they are saying.
"It is
colonialistic to not support ABC. ABC was developed by Africans for Africans
- we are supporting their strategies."
Speaking to
the BBC, Mr Lewis said the West had failed to provide sufficient funds to
finance effective long-term prevention and treatment programmes.
"The G8
countries could help to break the back of this pandemic if they viewed it as
an emergency like no other emergency - as the worst scourge on the face of
the planet since the Black Death of the 14th century.
"That sense
of urgency is not yet evident."
$332-billion illicit drug
trade fuelling HIV infections around world: expert
TORONTO -
The illicit drug trade is fuelling HIV-infection rates in many parts of the
world - and too much reliance on punitive drug enforcement is compromising
efforts to prevent spread of the disease, the International AIDS Conference
was told Tuesday. Australian physician Alex Wodak said that one in every 10
new HIV infections around the world occurs among injection drug users, and
they are responsible for about 30 per cent of new infections outside Africa.
"And the
proportion of global HIV infections attributable to injection drug use are
growing," said Wodak, director of the Alcohol and Drug Service at St.
Vincent's Hospital in Sydney.
"Drug use
around the world is also a growing problem that the war on drugs has
completely failed to arrest," he said, noting that the UN Office on Drugs
and Crime estimates that the drug trade has an annual turnover of more than
$322 billion US a year, which accounts for eight per cent of total
international trade.
A recent
report to British Prime Minister Tony Blair and his cabinet estimated that
between 26 and 58 per cent of that business is pure profit, he added.
"So this is
what's fuelling the epidemic of HIV in injection drug users worldwide. And
we're now seeing drug use spreading into Africa."
Wodak said
harm-reduction experts have known how to prevent HIV infection in IV drug
users for at least 15 years, by educating drug users, providing clean needle
syringe programs and getting "dirty equipment out of circulation."
There are
also a range of drug rehabilitation programs, notably methadone for heroin
users, that have proven successful, he said.
The major
barrier to stopping the spread of HIV in drug users is "excessive reliance
on drug enforcement" around the world, particularly in high-incidence
regions such as central and eastern Europe and central Asia - "where the
epidemic among injecting drug users is of alarming proportions," he said.
Wodak said
the United States has the highest incidence of AIDS in the industrialized
world, roughly five times greater than second-place Spain, in part because
of its failure to control HIV among injection drug users.
"Yet the
opposition in the United States prevents these pragmatic approaches being
spread throughout the world." While progress is being made in the fight
against HIV/AIDS, the disease is still spreading faster among injection drug
users than harm reduction programs needed to slow transmission, he said.
"And I find
it particularly galling and tragic in that this is one part of the epidemic
we really could do something about," Wodak said, "and yet it's the politics
in so many countries that prevents us from doing what has to be done."
Continuing
on the topic of harm reduction - a widely used buzz word at the conference -
a leading scientist said Tuesday that researchers are looking beyond the
famous ABCs of HIV-prevention.
The ABCs
stand for abstinence, being faithful to one sexual partner, and using
condoms.
Gita Ramjee,
director of the South African Medical Research Council's HIV Prevention
Research Unit, is involved in numerous trials of HIV-killing microbicide
gels and other prevention tools in the battle against HIV-AIDS.
"I have
described a new acronym that goes right up to I," Ramjee told a news
conference.
"We have an
additional C for circumcision, D for diaphragm for HIV prevention, E for
exposure prophylaxis - both pre-and post - F for female-controlled
microbicides, G for genital-tract infection, H for HSV-2 suppressive therapy
and I for immunization through vaccine.
"We have to
believe that we are getting to I," she said.
Recent
studies have found that treatment of herpes simplex virus HSV-2 infection
appears to reduce levels of HIV in the genital tract and blood plasma.
Dr. Helene
Gayle, co-chair of the conference, said some of the approaches discussed by
Ramjee may be effective against HIV within the next few years.
"However,
there are major hurdles facing new prevention approaches . . . in conducting
clinical prevention trials," Gayle said.
Among them
are finding groups of people for testing who are not yet infected and
deciding what to do if a person sero-converts (develops HIV-infection)
during a trial, she said.
Supporters of Vancouver's
safe injection site turn up the heat on Ottawa
TORONTO -
Supporters of Vancouver's safe IV drug injection site turned up the heat on
the federal government Tuesday, telling a news conference at the
International AIDS Conference that closing the site is not an option.
Advocates
say the facility, called Insite, has decreased public injecting of drugs,
saved lives and led to a decrease in petty crime in Vancouver's Downtown
Eastside, the inner city neighbourhood known for its high concentration of
injection drug users. But they fear the new Conservative government has
moral objections to the site and may be poised to close it.
"If we're
really taking a moral position . . . it would be immoral to ignore the (scientific)
evidence to date," said Dr. Thomas Kerr, a researcher with the B.C. Centre
for Excellence in HIV-AIDS, which has been evaluating the pilot program
through a series of scientific studies. A number have been published in the
world's leading medical journals, including the New England Journal of
Medicine.
The
director of the centre for HIV-AIDS was more blunt.
"Let's just
be clear. This is not about evidence," said Dr. Julio Montaner, an
internationally renowned AIDS researcher who is about to become
president-elect of the International AIDS Society.
"So
whatever the government is currently considering has to be something. And
it's up to them to tell us what they're looking at. We haven't been able to
figure it out."
Insite
operates under a legal exemption that expires on Sept. 12. Supporters of the
project find the federal government's silence on its future increasingly
ominous.
"I'm very
concerned this will become a political decision. We need this to be a
health-based decision," said NDP MP Libby Davis, who represents the area in
Parliament.
"I'm very
concerned about the chaos if it is closed down. It does bring a measure of
stabilization to the community."
"The site
is not contributing to increased crime or new cases of addiction; it is
controlling the spread of HIV because addicts have access to clean needles
and is in fact encouraging them to seek treatment," Liberal Senator Larry
Campbell, former mayor of Vancouver, said in a release in which he and
Liberal health critic Ruby Dhalla called on the federal government to keep
Insite open.
It is
estimated the safe injection site serves between 4,000 and 5,000 injection
drug users drawn years ago to the Downtown Eastside, where a large number of
rooming houses offer cheap accommodation.
The
concentration of so many injection drug users in a few city blocks led to
enormous social problems, with drug users shooting up in alleys and high
rates of petty crime in a neighbourhood that borders the city's very popular
Chinatown.
Studies
conducted by Montaner's researchers point to decreases in car break-ins,
fewer overdoses that lead to death, less syringe sharing and less shooting
up on the street.
The
researchers say the results have been so positive that people who initially
objected to the pilot project - local merchants, the Vancouver police - are
now firmly on side.
"So if the
police department can see it, if the business community can see it, if the
residents of the area can see it, if the city of Vancouver can see it, what
is there that you cannot see, Mr. Prime Minister?" Montaner asked at the
news conference.
While
experts believe the facility could reduce the risk of the drug users
becoming infected with AIDS by providing clean needles, the three-year pilot
project hasn't been long enough to assess that scientifically.
But
Montaner said on every other criteria measured, the site is reducing risk to
the addicts who use it, pointing more of them towards rehabilitation
programs and improving life in the city's core.
"The site
has already proven itself of value in terms of treatment of overdoses,
treatment of infections, referrals to detox, increasing public order,
preventing bad outcomes in these individuals. What else do we need to
justify continuation?" he asked.
"When you
do a test in Canada, it's to find out if something works or it doesn't work.
OK, the answer is it works. What do we do from here? And closing it is not
an option."
A woman
representing the drug users in the area said she knows what to expect if
Insite's doors close next month.
"I start
going to a lot more funerals again," Diane Tobin, a representative of the
Vancouver Area Network of Drug Users, told the news conference.
Male
circumcision not an easy answer for HIV
Mention adult male circumcision in conversation in Canada, and the
response from most men is a wince, maybe even an involuntary protective
hand movement toward the midsection. But there's a six-month waiting list
for the operation in Swaziland today — because there, in the country with
the world's highest rate of HIV infection, men have heard that having
their foreskins removed may protect them from the virus.
Other countries
could soon have Swazi-style waiting lists: circumcision was the hot topic
of the day at the international AIDS conferences yesterday, when a variety
of researchers and even former U.S. president Bill Clinton endorsed it as
an effective way to stop the spread of the disease.
No question, the
numbers seem to suggest it's worth doing. AIDS experts have speculated
about this for years, noting that the rates of HIV infection are much
lower in places where all men are routinely circumcised.
The first definitive proof came a year ago when a randomized trial in the
South African township of Orange Farm was halted early because the data
showed that circumcision gave men who had the procedure a 61 per cent
protection rate for infection, compared to men who didn't. Researchers
said they couldn't in good conscience keep the trial going without giving
the uncircumcised men the chance to get the operation and get protected.
New data
presented yesterday compared nearly 2,000 men in Kenya, some circumcised and
some not, and found the rate of new HIV infection to be roughly two-thirds
higher among the uncircumcised men. Another study found that if 20 per cent
of adult men in the South African township of Soweto were persuaded to have
the surgery, it would prevent 53,000 new HIV infections over 20 years.
“Even
modest programs can convey substantial health benefits and should be
implemented immediately,” epidemiologist Kyeen Mesesan said.
Now all
eyes are on trials underway in Kenya and Uganda, from which data will be
available next year. Should they show results similar to those in Orange
Farm, the United Nations may begin to recommend male circumcision as a
crucial health intervention much like polio vaccination.
Circumcision lowers the risk of HIV infection because the skin that is
removed contains more of the cells to which HIV easily attaches — it cuts
off the sticky bits, essentially.
The problem
is that adopting male circumcision as a public health measure to stop HIV
infection brings with it a great, swampy mess of problems — and those got
short shrift in the fervent discussions about the science yesterday.
Circumcision is, of course, much more than a medical procedure. For Muslims
and Jews, it's a religious rite. For many of the cultures of east and
southern Africa, it's a hugely important marker of boys' transition into
manhood. But in cultures that don't circumcise males, that decision is often
equally sacrosanct.
How is the
World Health Organization, or national governments, going to persuade people
to, first, start doing it, if culturally they are non-circumcising people? (Roughly
half of African societies routinely circumcise at some point in a man's
life.) Second, how do you persuade a society with an elaborate ritual for
17-year-old boys to instead start circumcising infants, on whom it's a much
easier operation with far fewer possible complications? Another big concern
is that, once circumcised, men will believe their level of risk is so low
they won't use condoms (when of course the operation offers no such total
immunity) or that youth, hearing about the practice, will get the mistaken
impression that they do not need to take precautions, although a study from
Kenya presented yesterday found that essentially there was no increase in
risky sex among men who were circumcised.
“Is this
going to take resources from other known HIV-prevention interventions — will
it be taking resources that maybe could be employed in better condom
promotion or education?” mused Tim Farley, who heads the sexually
transmitted infection control team for the World Health Organization.
The Swazi
waiting lists suggest that it's not necessarily difficult to persuade adult
men to get the operation. But other acceptability studies in Africa have
shown that less than half of men are willing.
TORONTO
-- In the heart of Toronto yesterday, the AIDS message pierced the heart
of the growing epidemic.
Young
designers and models from India, China, and Canada showcased AIDS-themed
fashion on the runway at Yonge-Dundas Square, drawing a large crowd of
people aged 15 to 24 -- the same age group currently seeing more than 50
per cent of new HIV infections around the world.
"Incorporating
fashion into the fight against AIDS will really get to us. I know it's
getting to me," said 18-year-old Moraa Saisi in the audience for the
show put on in partnership with YouthCARE.
Ms.
Saisi, who was born in Kenya but grew up in Toronto, said she has been
struggling to communicate the importance of HIV-AIDS to her friends. She
hopes T-shirts such as the ones displayed yesterday with slogans reading,
"We can all be heroes to end AIDS" and, "Stop the spread. Get tested,"
will catch on so that the message spreads faster than the disease.
The
loudest cheers went to Toronto's Tiffany Aita, who wore a black satin
gown with a wide, red silk ribbon tied around her neck like a halter and
crossed in front to represent an AIDS ribbon.
"Fashion is what youth are interested in, so if you can get to them with
clothes that people are going to ask about, you'll be successful," said
the 17-year-old who will be entering the fashion-design program at
Ryerson University in the fall. To illustrate her point, she referred to
the buying craze that erupted last year after actor Ryan Gosling wore a
"Save Darfur" shirt to the MTV Movie Awards.
Microbicides a new champion in
AIDS fight
TORONTO
— With the search for an AIDS vaccine proving elusive, scientists and
activists are increasingly pinning their hopes for slowing the epidemic on
microbicides, easy-to-apply gels that would act as an “invisible condom” to
prevent infection.
“The
prospect of a microbicide is thrilling,” said Stephen Lewis, United Nations
special envoy for HIV-AIDS in Africa. “Regardless of its effectiveness, it
will inevitably save millions of lives.”
In fact, a
recent study conducted by the London School of Hygiene and Tropical Medicine
estimated that a microbicide that reduced the risk of infection by 40 per
cent — and that was used by 30 per cent of women at risk in low-income
countries — would avert more than two million HIV infections a year and save
$1-billion (U.S.) annually in health-care costs.
Gita Ramjee,
director of the HIV-AIDS program at the South African Medical Council, said
it is impossible to overstate how desperately women — who make up
three-quarters of new infections in sub-Saharan Africa — need some form of
protection.
They do not
know if they will be infected tonight, tomorrow night or the next night. The
threat is always there,” she said.
Worldwide,
an estimated 38.6 million people are infected with HIV-AIDS, half of them
women. The epidemic is spreading fastest among young women aged 16 to 24.
Condoms are
an effective means of blocking transmission, but condom use is low. In much
of the world, women do not have the power — physical, legal or social — to
negotiate safer sex. They must succumb to sex when, where and how their
partner chooses, even if that partner is HIV-positive.
Microbicides can be packaged in a gel, foam, vaginal ring, sponge,
suppository or douche form. Scientists are hoping to develop products that,
in addition to blocking the transmission of HIV-AIDS, will prevent other
sexually transmitted diseases such as herpes, gonorrhea and chlamydia and,
in some cases, also have contraceptive properties. Unlike other forms of
protection such as condoms and cervical caps, they also hope to produce
products that are long-lasting, able to thwart the virus for days, or even
months.
“Women need
multiple drugs with multiple delivery options,” said Zeda Rosenberg, chief
executive officer of the International Partnership for Microbicides, a group
based in Silver Spring, Md.
She said
that variety in microbicides is essential because, like birth control,
“women have different needs at different stages in their lives.”
Currently,
there are dozens of microbicides in development, but five are at a fairly
advanced stage, and being tested in humans. One of these, called C31G (brand
name Ushercell), is Canadian, and being produced by Polydex Pharmaceuticals
Ltd. Results of the first studies will be published late next year, and the
product could be on the market by 2009.
Microbicides work in various ways. Some, such as Carraguard, a seaweed-based
gel, create a physical barrier that keeps HIV from reaching cells where they
will latch on and infect a person; others, like Ushercell, which is derived
from cotton, disable the virus by stripping off its outer covering. Another
class of microbicides boosts the vagina's natural defence mechanisms by
raising pH levels and creating an acidic environment hostile to viruses.
The key is
finding out whether the products, which work in the lab, will be effective
for people living everyday lives.
There are
concerns that the advent of microbicides will be seen as a substitute for
safer sex practices such as condom use, and that the products will be
shunned because of a belief they prevent pregnancy. (Scientists stress that
both contraceptive and non-contraceptive microbicides will be developed.)
Alex Coutinho, executive director of the AIDS Support Organization of Uganda
(TASO), said the science of blocking is the easy part. The hard part is
creating products that women will actually use and that are affordable and
readily available.
“It's not
just about microbicides, it's how you deliver microbicides that really
matters,” he said. “Women need something they can fit and forget.”
A fine balance between
rights and successful HIV testing
Not
long ago, a weary nurse named Violet led me on a tour of a hospital ward
in Morija, Lesotho. Every bed but one held a gaunt woman with tuberculosis,
pneumonia, herpes zoster and festering abscesses. Any five-year-old in
Lesotho could have told you these women had AIDS.
I asked Violet,
quietly, if any of them had been tested for HIV. She shook her head. “So,”
I said, “Will you offer them tests now?” She shook her head much harder.
“Oh, no,” she said. “We don't do that.”
The women hadn't
gone for HIV testing themselves, although they almost certainly knew what
they had, because of all the fear and shame that comes with AIDS. And the
nurses weren't going to do it either — Violet flinched every time I said
“HIV.” On the ward, they refer instead to “immune suppression.”
This business of testing is one of the great conundrums of AIDS, something
people are wrestling with all over Africa, and the debate erupted again at
the International AIDS Conference yesterday. Human-rights activists are
alarmed by the new trend in the field: routinely offered testing, which
they fear is a slippery slope toward mandatory testing. But Violet, and
her ward of untested women, suggest something has to give.
The current
standard practice, recommended by the World Health Organization, is what's
called voluntary counselling and testing (VCT). People must present
themselves to testing sites and undergo both pre- and post-test counselling
about HIV.
It is a
legacy of the early days of the AIDS epidemic in North America, when the
disease was first recognized among gay men and intravenous drug users — who,
as marginalized groups, needed the promise of confidentiality, or often
anonymity, to be persuaded to be tested. This culture of delicately handled
testing was exported to Africa and the rest of the developing world; it is
viewed as a human-rights violation to test a person for HIV without express
consent.
But in
recent years some of the major figures in public health have been arguing
that VCT is a mistake. AIDS, they say, is a disaster, and relying on
volunteerism in the face of a stigmatized disease is madness. Look how
Canada handled SARS. You weren't asked to volunteer for a test when you
stepped off that flight from Hong Kong, now were you?
Yesterday,
Botswana's formidable Health Minister, Sheila Tlou, explained that in 2004
her country had a problem. Botswana, where one in three pregnant women tests
positive for HIV, has a strong health system and was the first country in
Africa to offer free AIDS treatment. Despite that, very few people were
volunteering for tests.
That made
sense when there was no treatment; what's the point of being tested for a
fatal illness if you'll just be sent home to die? But testing numbers barely
crept up once the drugs were widely available.
So in early
2004, Botswana's government decided instead to introduce a “routine offer of
testing.” Everyone who comes into contact with the health system is offered
an HIV test, and the onus is on the patient to decline.
Ms. Tlou
said the policy has been a success; it has nearly tripled the numbers of
people who are tested, and receive treatment, and helped to lessen the
stigma around AIDS by making it less of an “exceptional” case. Now you get
an HIV test like an allergy test.
But the
minister faced off yesterday against an array of human-rights activists who
say the routine testing policy has substituted one problem for another.
Women in Botswana have great difficulty, culturally, rejecting the
suggestion of a person in authority, said Grace Sedio, an activist living
with HIV. They'll be tested when they don't really want to, when they aren't
ready for the news or may face violence at home if they disclose they have
HIV. They certainly won't embrace “positive living” or a complicated
treatment regimen if they aren't ready, she said. Others raised the fear
that the goal of routine testing is primarily to produce numbers to show
donors that progress is being made.
While it's
not fashionable these days to champion routine testing, many African
health-care workers will tell you quietly that making the test standard
policy (with, of course, an opt-out) is the only way to get over the fear.
Sick people assume their doctor or nurse will suggest an HIV test if they
see the possibility of infection, one Zimbabwean doctor told me yesterday.
“And you can't say that because a woman is poor and African, she is not
capable of truly consenting to a test she is offered,” she added.
Genetic mutation acts as
a shield
Why do some HIV patients
fare better than others?
In the 25
years that Ron Rosenes has lived with HIV, he has always suspected
something more than good fortune shielded him from the worst of the
disease.
Mr. Rosenes feels
he contracted the AIDS virus before anyone knew it existed and "safe sex"
became the mantra of a generation. "I was sexually very active in the late
seventies," he said.
He has lost
several friends and a close cousin to AIDS. In 1990, he watched his
partner of 15 years die in the home they shared.
But even as he lost weight, left his job and
made do with the "sub-optimal therapies" of the early nineties, Mr.
Rosenes held on.
He never
suffered the opportunistic infections others endured. He never picked up
anything life threatening. Although his viral load soared and certain immune
cells plummeted, blood test after blood test showed a healthy presence of
other immune cells.
"It became
more obvious to me, especially after [my partner] died, that I was being
spared."
The
59-year-old Toronto man may well have his family history to thank. Mr.
Rosenes carries a gift in his genes — a mutation that confers a natural
resistance to HIV. In all likelihood, it was passed down to him from his
ancestors in Europe, where the protective trait is most prevalent.
From the
earliest days of the epidemic, doctors have puzzled over long-term HIV
patients who show little progression from infection to full-blown AIDS. Some
have never had to take even a single drug to keep the virus in check. Others,
despite repeated exposure, have never contracted it.
The
question now is whether their good fortune truly is inherited.
The
mutation Mr. Rosenes carries is the best-known example of genetic resistance
to the AIDS virus. It offers not immunity, but a form of protection
that drug makers are keen to mimic. But there are most certainly other
genetic traits that confer resistance or susceptibility to HIV, and the race
to find them has begun in earnest. An effective treatment, perhaps even a
vaccine, hangs in the balance.
In the
United States, two separate research groups have recently identified traits
linked to HIV susceptibility. Scientists at the British Columbia Centre for
Excellence in HIV/AIDS are recruiting HIV patients considered to be "long-term
non-progressors" who have never actually developed AIDS.
This spring,
an international consortium of universities launched an ambitious project to
scan the whole genomes of hundreds of HIV-positive Europeans and Africans
for mutations that might be linked to the disease. Some scientists even
suspect genes may partly explain why HIV has hammered certain regions more
than others, sub-Saharan Africa in particular.
"My
hypothesis is that there are biological differences in susceptibility, and
knowing them will be crucial for the development of a vaccine," said Jacques
Pépin, a professor of microbiology and infectious diseases at the University
of Sherbrooke. "If we don't know why some people get infected and others
don't, why some people get sick and others don't, we'll never understand how
the virus works or how to stop it."
Mr. Rosenes
has made good use of his time. He's been chair of the AIDS Committee of
Toronto, a board member of the Canadian Treatment Action Council and the
willing subject of research.
In the
mid-nineties, he submitted his blood for an experiment at McGill University
investigating ways to boost the immune system. Not long after, the lab
called to tell him about the protective quirk they'd found in a gene called
CCR5.
"I really
found out about it in a fluky kind of way," Mr. Rosenes recalled.
CCR5 is a
gene that produces tiny keyhole-like entry points on the surface of the
immune system's T cells. They're known as chemokine receptors. HIV, like a
savvy burglar, happens to have the right set of molecular keys to unlock
them and break into the cell to cause infection. There are about 23
different mutated versions of the CCR5 gene. But the most common and best
understood is one called CCR5-Delta32. People with this mutation have 32
bits of genetic code deleted in the CCR5 gene. The missing bits result in
fewer entry points on the cell surface, upping the chances of shutting out
HIV.
People who
have one Delta32 copy — as Mr. Rosenes does — have partial resistance, with
a two- to four-year delay in the progression of HIV. Those who inherit two
copies of the Delta32 mutation — one from mom and the other from dad — have
almost absolute protection.
"If they
have one copy, we call them lucky. If they have two copies, we call them
really very lucky," said Richard Harrigan, director of the research lab at
the B.C. Centre for Excellence in HIV/AIDS.
Mr. Rosenes,
vice-chair of the Local Host board of directors of the 2006 International
AIDS Conference in Toronto this week, feels that his mutation "helped to
bridge the gap" between the time he contracted the disease and when
effective drugs became available in 1996.
"I
understand it as a key factor in my long-term survival," he said.
Since its
discovery in 1996, studies have piled up showing the protective mutation is
more common in certain places in the world. In Europe and West Asia, the
prevalence rate runs as high as 10 to 15 per cent, and the numbers rise the
farther north you go. In Southern Europe, it's roughly 4 per cent or less. A
1998 study that tested 2,500 people from 16 European countries found the
highest frequency in Denmark and the lowest in Corsica.
One per
cent of Caucasians are estimated to have the two copies that confer
near-immunity to HIV. In particular populations, such as Ashkenazi Jews of
Eastern Europe, a group that includes the ancestors of Mr. Rosenes,
estimates peg the rate as high as 15 per cent. But in native Indians, East
Asians and people in sub-Saharan Africa, home to two-thirds of the world's
AIDS cases, the mutation is rare to non-existent.
To Dr.
Pépin, the pattern supports his view that certain populations face a higher
biological risk of contracting HIV.
"Everybody
in the field knows the prevalence in Africa is higher than the rest of the
world," he said. HIV rates in parts of sub-Saharan Africa are higher by
400-fold compared with Scandinavia, he noted.
Most people
accept that most of the gap can be explained by socio-economic differences
that have nothing to do with DNA, said Dr. Pépin, who worked in Africa
during the 1980s. These include the region's poor state of nutrition and
lack of access to hygiene, health care and education. The urbanization of
Africa has also brought men to the cities, leading to more transient sex,
more commercial sex and a higher prevalence of other sexually transmitted
diseases. All of these things increase the risk of spreading HIV.
"If you
look at a map of the world, you see the regions with the highest prevalence
are sub-Saharan Africa and the Caribbean, places where there are populations
who came from Africa as slaves," Dr. Pépin said.
To
investigate this, Dr. Pépin decided to look at a place of mixed populations
and determine if there was any correlation between a person's geographical
ancestry and HIV prevalence. He picked 34 countries in the Americas,
including Haiti, largely populated by descendents from sub-Saharan Africa;
the Dominican Republic, with its blend of Spanish, European and African
descendants; Cuba, with a 10 per cent African and 30 per -cent mixed
European population; and Argentina, which imported relatively few African
slaves.
He then
relied on HIV prevalence rates in the countries of origin to predict the
prevalence rates among population groups in the countries of mixed
populations — and they closely matched.
"What I
observed is not due solely to behavioural factors," he said of the work,
published last summer in the journal of Tropical Medicine and International
Health.
The
pattern, he pointed out, is also what you might expect to see when something
like a CCR5 protective mutation is present at such low levels in one
population and higher levels in another.
"But there
is not a single factor that explains it all," he said.
The CCR5
gene mutation sprung up as most do: a one-time, random event in a single
person. Initially, scientists thought it happened fairly recently, popping
up just 1,000 years ago and then spreading rapidly across Europe, helped by
the Viking raids of the 8th to 10th centuries, but more so because the
mutation offered some form of a survival advantage.
"There must
have been some kind of an epidemic in Europe, which extended to North
Africa, that wiped out the people who [did not have the mutation]," Dr.
Pépin said. "It's possible that populations in Africa suffered a little bit,
but maybe [that epidemic] didn't reach portions of sub-Saharan Africa."
A number of
candidates have been suggested: the bubonic plague, typhus, influenza. But
to Montgomery Slatkin, a population geneticist at the University of
California at Berkeley, none of these fit the bill.
These
historical infections, he explained, did not result in enough deaths in a
short enough time period to change the frequency of the CCR5 gene type to
such an extent.
Dr. Slatkin
and his team constructed a mathematical model of the mutation's spread and
concluded smallpox was the likely candidate. The highly contagious virus
killed up to 40 per cent of its victims in Europe during the Middle Ages and
hit the continent's northern countries especially hard.
But
scientists now suspect the mutation may be much older than originally
thought. German researchers discovered it in the DNA of 2,900-year-old
Bronze Age skeletons and in the remains of people who died of bubonic plague
in the 14th century. Further genetic analysis also suggests it may be 5,000
to 10,000 years old.
Given these
findings, Dr. Slatkin said a number of factors could have contributed to the
spread of the protective mutation in Europe. But the smallpox epidemic, he
said, "remains a plausible explanation" for its relatively high frequency in
Europe.
In fact,
Dr. Slatkin estimates that if AIDS continues its deadly spread in Africa,
the resistant trait could soar from near zero in the southern part of the
continent to as high as 10 per cent in 200 years.
When Sunil
Ahuja entered the arcane world of immune-system receptors in the early
1990s, it was, he says, "a sleepy field." But after CCR5's role in HIV was
uncovered a decade ago, "there was a stampede."
Yet Dr.
Ahuja, now an HIV researcher at the University of Texas Health Science
Center at San Antonio, points out that a raft of other traits, both in and
around the CCR5 gene, deserve attention.
"People
have tended to focus just on this," Dr. Ahuja said, "but what about all of
its other partner [mutations]?" Dr. Ahuja, collaborating with
Lieutenant-Colonel Matthew Dolan of the U.S. Air Force Wilford Hall Medical
Center, turned his eye to the genes that produce chemokines.
Since HIV
locks on to chemokine receptors as its "kiss of entry" into a cell, he
decided to investigate the genetic production of chemokines — molecules the
body makes naturally to lock on to that same entry point. A gene called
CCL3L1 does exactly that.
When Dr.
Ahuja and Col. Dolan analyzed blood samples of more than 4,300 HIV-negative
and HIV-positive people of different ancestral backgrounds, they found an
astonishing thing: The human genome has mysteriously stockpiled extra copies
of this gene.
Some
individuals carry as many as 10 to 15 copies of the CCL3L1 gene (generally,
people have been thought to inherit two copies of a gene, one from each
parent). People of African descent, Dr. Ahuja said, were found to have on
average six copies; Hispanics, three and Europeans, two. The study,
published in Science in March of 2005, found the fewer copies of this gene
people have, the more susceptible they are to being infected after having
unprotected sex with someone who is HIV positive.
This is
because with extra genes, the body throws so many of its own molecules at
the CCR5 entry point, it gums up the lock and makes it tougher for the AIDS
virus to break through, Dr. Ahuja explained.
From this,
you might assume Europeans are more prone to HIV infection since they have
fewer copies of this blocking gene than African populations. But the
researchers found that the risk was relative to a person's population — it
increased if you had fewer copies than other people in your ethnic group.
African
Americans were found to be more susceptible to HIV infection if they had
fewer than four copies of the gene. Hispanics were at greater risk if they
had fewer than three copies and Europeans if they had less than two copies.
"What we
see here is a gene dosage effect," Dr. Ahuja said. "The more genes, the more
protection."
Having
below the group's average number of genes significantly increased the risk
of getting HIV — and the chances of having rapid disease progression. That
risk may be even higher if there is a low number of the CCL3L1 gene and the
riskier, unmutated form of CCR5.
"The point
is that this is going to be a very complex story," Dr. Ahuja said. "There
are many questions yet to answer."
Researchers
face three major hurdles in finding genes linked to HIV infection. First,
doctors don't often come across patients like Mr. Rosenes, who appear to
have a natural, if partial resistance to HIV. In B.C., Dr. Harrigan said the
trial studying long-term non-progressors has yet to recruit any patients.
Without the
big numbers of a large study, it can be tricky to tell when a trait is
important or just a personal quirk.
Nor is
there any simple way to factor in all of the environmental and behavioural
forces that affect a person's risk of contracting HIV.
Even Dr.
Pépin admits that his study predicting HIV prevalence in mixed populations
is limited by its inability to completely take environmental or behavioural
factors into account.
Third, it
has been difficult to know exactly where in the genome to look for traits
that might confer resistance or susceptibility.
But the
newly formed Center for HIV/AIDS Vaccine Immunology (CHAVI), a consortium of
universities and academic institutions around the world, has this year
launched a massive study it hopes will overcome these issues.
"We have
these beautiful machines [for DNA analysis], and the money that the Gates
Foundation has given to us, and we have had no people [to study]," said
Amalio Telenti, an HIV researcher at the University of Lausanne in
Switzerland who is working on the project.
But CHAVI
has in fact just recruited 600 Caucasians from Europe and Australia who have
all contracted HIV within the past decade. Researchers have access to their
personal histories and medical files, and plan to scan half a million
genetic mutations in each subject.
Dr. Telenti
said the team is using the mutations set out in the Haplotype Map. That map
is the first catalogue of the different genetic mutations found in four of
the world's major populations — European, Chinese, Japanese and Nigerian.
Once this
is complete, the second round of the project will focus on Africans or
people of African descent, Dr. Telenti said. He then hopes researchers in
other countries will use their approach to scan the genomes of other
populations.
But while
they are studying groups by ancestral background, Dr. Telenti said he does
not expect to find major HIV-response differences between populations.
Rather, he
said, it will more likely be the subtle effects of a number of traits.
"No one is
looking for a miracle gene, but to help find targets for antiretroviral [agents],"
Dr. Telenti said. "We need to understand the basis of susceptibility, and to
what extent genes can explain that."
For Mark
Wainberg, director of the McGill University AIDS Centre in Montreal, the
hunt for genes that affect a person's response to HIV is well worth it,
since it may lead to more effective therapies.
"Finding
the mutation in CCR5 has already led to efforts to make a drug to block this,"
he said. "The thinking is, if there are healthy people walking around out
there with deleted copies of this gene, then it would be a safe target for a
drug."
As well,
genes are already known to influence the way people respond to drugs, an
issue that is becoming more urgent in the face of growing resistance to
current antiretroviral therapies.
But Dr.
Wainberg, co-host of this week's International AIDS Conference, also worries
that people who believe they carry some form of genetic protection against
HIV will become complacent: "It doesn't matter if you have one copy or two
copies [of a gene], you should still have safe sex," he said.
Research
suggests he has good reason to worry. A 2001 study found a correlation
between gay men who carry two copies of the protective CCR5 mutation and an
increase in risky behaviour.
Dr. Ahuja
saw himself how the public might overestimate the power of genes to protect
them from infection. When he once told The New York Times that two copies of
the CCR5 protective mutation was like a "genetic condom," his voicemail
clogged up with people wanting to know where they could buy it.
The smartest virus in
history?
Tracing the origins of HIV has been a Herculean task and often not a
glamorous one. Most recently, it involved the serious scrutiny of 599
samples of ape feces.
But after two
decades of work, scientists have slowly pieced together a biography of the
human immunodeficiency virus — where it was born, what its ancestors were
and possibly how it grew up to be the mass murderer of the modern era.
Not since the
Middle Ages has one virus cut such a long, wide swath through humanity.
More than 25 million people have died since HIV was first recognized in
1981. More than 40 million have been infected. Some experts predict that
by 2020, AIDS could prove to be the most destructive pandemic in history.
Yet in all likelihood, HIV was not the first virus of its kind to infect
humans, and scientists suspect it will not be the last.
The closest ancestor of the AIDS virus lived in West Africa's chimpanzees
for thousands of years, and chimps have long been on the menu of human
hunters in that corner of the world.
"Our guess
would be that these viruses have been jumping from chimps into humans on
countless occasions in the past," said Paul Sharp of the University of
Nottingham, a leading expert on HIV's evolution. "But most of them don't
make it to be an epidemic. In fact, until recently, none of them had made it
out of rural areas or infected enough people to be noticed."
HIV is
believed to have been killing people in Africa for roughly 50 years before
the world knew the virus existed. Yet scientists have since discovered the
pandemic virus was one of three types of HIV that jumped to humans around
the same time. But due to a fateful confluence of events and genetic
accidents, only the one — HIV-1, group M — gave rise to the global scourge
that continues to stump medical science.
The king of freeloaders
HIV belongs
to a group of pathogens known as retroviruses. They were once considered
rare, medical curiosities and only late in the 20th century were they
discovered to actually infect humans.
They have
no ability to replicate outside of a host cell and they carry their genetic
material not in the double-stranded code of DNA, but the single strand of
RNA that makes proteins.
HIV is a
retrovirus with just nine genes tucked inside a round protein envelope.
Magnified, it looks a little like the wheel of a ship, circular with spikes
radiating from its surface. The virus makes its way through the world on
rivers of bodily fluids, striking humans at their most intimate points of
contact — sexual intercourse, childbirth, breastfeeding. Tainted blood and
intravenous drug use have also been sources of transmission, and HIV has
developed uncanny methods to spread itself. Outside of a human host, it's
powerless.
"It's a bit
wimpy that way," said Richard Harrigan, director of the research
laboratories at the B.C. Centre for Excellence in HIV/AIDS. A few hours
outside of a human body and the virus is no longer infectious, he said; nor
can it be easily grown in a lab dish.
But inside
a T cell, the story is dramatically different. T cells are lymphocytes, or
white blood cells, that orchestrate the body's ability to fight infection.
The HIV attacks them, specifically a type known as CD4, like a guided
missile.
The virus
breaks in with its own set of keys and slips into the host cell like an
unwanted guest. Then it settles down to become the king of freeloaders,
injecting its own genetic material into the DNA of its host and making an
HIV factory of the very cell that was designed to kill it.
New viruses
eventually burst out of the host cell to wreak fresh rounds of destruction.
"Integrating itself directly into the DNA of the host means you can't get to
it easily to cause its destruction without the risk of damaging the host's
cell," Dr. Harrigan said. "It also makes lots and lots of copies of itself
every single day."
How many
copies?
"Oh," he
said, "about 10 billion."
It started with chimps
Chimpanzees
had long been the suspected source of the AIDS pandemic. HIV bears a close
genetic resemblance to a chimp infection known as simian immune deficiency
virus, or SIVcpz.
But it was
only this spring that an international team of scientists, led by Beatrice
Hahn at the University of Alabama, was finally able to confirm that this
chimp virus exists in the wild and that it was indeed the progenitor of
HIV-1.
Dr. Sharp,
who, along with researchers in France and Cameroon, has worked with Dr.
Hahn's group since 1991, said the study, published in Science, was a long
time coming. Collecting blood from wild apes was considered too invasive and
dangerous, so researchers spent years developing molecular tests to run on
chimp droppings instead. The samples, amassed with the help of trekkers,
were scooped up from 10 remote areas of forest in central West Africa and
preserved in tubes.
Molecular
tests on the samples were able to determine the species and sex of the
animal to whom it belonged, whether it carried antibodies for an SIV, or
genetic material of the virus itself. The results showed the virus most
closely related to the HIV-1 pandemic strain was indeed the SIVcpz strain.
Researchers
believe it jumped to a single human from a chimp in southeast Cameroon about
70 years ago.
Scientists
can estimate the date because viruses are believed to mutate at a fairly
constant rate. By comparing the oldest known HIV strain with its progenitor
chimp virus, they can clock when the two diverged and one crossed the
species barrier.
"The only
missing part of the story is from one person [contracting it] around about
1930 or a little earlier, getting infected with the virus and then getting
it down to Kinshasa," Dr. Sharp said.
Kinshasa is
considered ground zero of the AIDS pandemic, since the HIV-1 subtypes there
are older and more diverse than anywhere else in the world.
"We would
imagine that this virus has been transmitted down rivers ending up in
Kinshasa, known as Leopoldville in those days," Dr. Sharp said. "The virus
needed to get to somewhere like that, it needed to get to a big city before
it could really get started as an epidemic."
The
earliest known case to come from the continent would not, however, be
diagnosed for several decades. A blood sample taken in 1959 from a Bantu man
participating in a medical study in Kinshasa was found in the 1980s to be
HIV positive. By then, the virus had the world's attention.
Mass cellular slaughter
Ask where
the AIDS virus ranks among its peer pathogens and scientists rarely hesitate:
"In terms of its smarts, it's right up at the top," said Mark Wainberg,
director of the McGill University AIDS Centre. "Not only does it know how to
escape from everything we throw at it, but if you're the virus, your main
objective . . . is to survive and spread yourself to as many people as
possible. You don't do that if you're a virus that kills your host within a
week. If you want to be efficient at spreading yourself, you want your host
to stay alive for a number of years and remain infectious throughout that
time."
In its
early stages, HIV triggers a mass slaughter of its host's T cells, most
notably in the gut. Tissues that line the intestines contain more
lymphocytes than any other single site in the body.
"This is
the largest organ in the body in terms of the immune system. If not the
heart, the soul of the immune system," Dr. Wainberg said.Scientists have
found it can take up to four months before the immune system kicks in to
produce antibodies that can be detected in a blood test.
"The immune
response you see with HIV is somewhat slower than what you see with lots of
other infectious agents," Dr. Wainberg said. "Probably because the immune
system is overwhelmed, partly because the virus is infecting the very cells
that we need to respond quickly. It's a very insidious virus."
The
earliest phase of infection is also the most contagious. With no immediate
immune response, the patient's "viral load" — the medical term for the
number of HIV particles in a given volume of blood — soars.
"Before a
person knows they are infected, they are at their most infectious and
because they don't know it, they are not practising safe sex," Dr. Wainberg
said.
Once the
immune system responds, the viral load drops, reducing the risk of
transmission. The viral load can remain low and stable for several years.
But that number will eventually rise again, resulting in big losses of T
cells that can lead to acquired immune deficiency syndrome without effective
treatment.
AIDS leaves
the body with an immune system so crippled that opportunistic infections,
such as pneumonia, tuberculosis and certain cancers pose a sudden and
serious threat. Yet one intriguing hallmark of HIV in humans is how few T
cells actually become infected. "At any given time, it's less than 1 per
cent," Dr. Wainberg said. "Yet the number of losses of T cells can be
profound."
Dr.
Wainberg said the accepted theory is that HIV not only kills the cells it
directly infects, but that infected cells secrete a substance toxic to other,
uninfected T cells. This in turn triggers the body's own killing of these
other cells.
Adapting to
new hosts
The
HIV-like virus chimps carry is a descendant of two other ape viruses — one
that infected red-capped mangabeys and another that infected Cercopithecus
monkeys.
"The
ancestors of those two monkey viruses have recombined to form what is now
the chimp virus [that gave rise to HIV]," Dr. Sharp said.
No one
knows exactly when chimps contracted it, but it's estimated to be anywhere
from 70,000 to 1.5 million years ago. Neither can anyone say how the virus
first affected chimpanzees. It may well have wiped out all chimps without a
natural resistance, Dr. Sharp said. "We know at the moment, these viruses
don't cause any illness in chimps. They get infected, but they never get to
the stage of deteriorating.
"The real
problem with AIDS is that you are destroying your own T cells, and when you've
destroyed your own T cells you are susceptible to infection. If somehow the
immune system can avoid recognizing the virus and destroying them, you may
be okay."
The chimp's
immune system, for example, has somehow learned to simply ignore the
infection, Dr. Sharp said.
Dr. Sharp
has lately been studying the three separate HIV-1 groups that jumped from
chimps to humans on separate occasions. His hope was to find something that
distinguished them from the chimp virus that spawned them.
"The logic
of our ongoing analysis was to say, well if we find a site in a gene which
is the same in each of the HIV groups, but different in all the chimp
viruses, then those are changes that have occurred in all of the three
groups leading to HIV," he explained, "that would be too big of a
coincidence for it to just be an accident. It must be something that has
been selected for as the virus adapts to its new host."
The hunch
bore fruit. Dr. Sharp has located a single chemical change in a protein
important to the core matrix HIV-1. The change is there in all three groups
of the human form of the virus, but not the chimp virus.
What's
more, Dr. Sharp learned that a research project 10 years ago showed that
when chimps are infected with HIV-1, the virus does not fare well. But over
time, the virus adapts and the protein switches back to the original form it
originally had in chimpanzees.
"This tells
you it's important for the chimp virus to have it one way, and to move into
humans to have it this other way."
Looking to
the future
People
often ask Dr. Sharp how it could be that a virus like HIV could go
undetected for half a century, infecting one person in 1930 to 40 million by
2000. But he's done the math, and he feels numbers as well as geography
explain it.
"If you did
just the simplest epidemiological plot . . . you see only about 2,000 people
infected in 1960. . . . Even by 1980, you are only getting up to a million
people.
"It takes a
long time for the numbers to build up. It really is not at all surprising
that nobody knew about this virus in 1960; there just weren't that many
people infected and they were all in Central Africa.
"So it's no
surprise to me that the virus went undetected for so long."
What
concerns him more is that about 30 species of monkeys in Africa carry simian
immune deficiency viruses. "With continued exposure to these viruses, more
of them could jump into humans," he said.
"There is
an ongoing risk."
The African state: an
AIDS survivor
Stanley Chinoya wants
nothing more than to go to school. He has mastered the alphabet up to E,
and he would like to learn the other 21 letters. But Stanley's parents are
dead; his exhausted grandmother, caring for him and another orphaned
grandchild, can't afford to send them to school.
Stanley
was born with HIV, which has left him, at age 10, half the size of other
children his age and chronically ill. So no one sees much point in
spending money on him. He is one of several hundred grubby orphans
loitering in the streets of his slum neighbourhood in this Zambian
copper-belt town.
At the
primary school Stanley cannot attend, there are 125 children in the Grade
2 class. Teachers keep dying and no one replaces them. Up the road, at
Kitwe Central Hospital, the medical wards are overflowing with patients
who all look the same: stick-thin, covered in lesions, gasping. Kitwe
Central is supposed to have more than 600 nurses. It currently has 245. At
the local Home Affairs office, people seeking passports or death
certificates sleep overnight in the doorway, hoping to be first in line
when the one or two remaining employees show up the next day.
In a
village half an hour's drive away, Buluma Ngusa finds herself raising five
grandchildren under the age of 5. At 69, she is twice the national life
expectancy. She had six children of her own; four of them have died in the
past two years. There is no one else left to work the family fields, so
she leaves at 4 a.m. to walk to the family plot. She grows about a quarter
of what the family had when her children were alive and able to work the
land.
"That's how
it is now, with the young people gone," she says. She has two sons left, but
one, Lakson, has been too sick to work since February. The other is off
trying to find a job at a sawmill. If he finds work, his wage will buy food,
but it won't extend to a trip into town, where Lakson could get an HIV test.
Things in
Kitwe are terrible. The situation isn't new, and to most of the world, it
isn't even that interesting. The intriguing question is this: In Kitwe, and
places like it, why aren't things worse?
In the late
1990s, as the world woke up to what AIDS was doing to Africa, international
agencies began to make increasingly alarming predictions. The World Bank and
United Nations pointed out that the disease was robbing sub-Saharan
countries of the precious development gains they had made over the previous
couple of decades -- that child mortality was rising, not dropping, that
life expectancies were in free-fall.
They began
to predict that the continent's frail economies would not only fail to grow,
but that they would contract as the most productive workers died. That
police services and militaries would buckle as their young, male ranks got
ever thinner. That gangs of unsocialized orphans would turn to crime and
violence. That people would starve as farmers grew too sick to work. That
governments, robbed of their civil servants, teachers and nurses, would no
longer function. That citizens weakened by illness or the demands of caring
for others would withdraw from public life.
Experts
began to predict the imminent collapse of the worst-hit countries.
Here's the
World Bank in 2003, commenting on South Africa, the continent's most robust
economy and the world's most-HIV-infected country: "If nothing is done to
combat the epidemic . . . a complete economic collapse will occur within
three generations."
And here's
Stephen Lewis, the UN Special Envoy on HIV-AIDS in Africa, in 2002: "I
wouldn't discount the possibility, 10 or 15 years down the road, of failed
states."
The phrase
"failed states" evokes images of a country in complete anarchy. But
sometimes states fail more quietly, when they cease to be able to provide
any level of services to their people, or to control their territory in
anything but name. This sort of collapse began to seem particularly
plausible in southern Africa, where three countries have HIV-infection rates
approaching half the adult population and even those qualifying as "better
off" have one in four adults infected.
To a great
degree, many of the worst predictions have come true. By 2004, troop
strength in Malawi's military had fallen below 50 per cent of what the
government said was needed to maintain national security. In Botswana, life
expectancy declined by about 30 years, to 35, between 1990 and 2004.
Africa's share of world trade declined from 6 per cent in 1980 to less than
2 per cent in 2002. Africa is the only region of the developing world where
food production fell over the past 20 years.
Botswana
(37 per cent HIV prevalence), Swaziland (43 per cent) and Lesotho (39 per
cent), all of them tiny countries with populations under 2 million people,
seemed marked for dissolution. Even larger countries seemed to be at risk.
Zambia, for
example. Although it has 11 million people, fertile land and mineral wealth,
Zambia has always been one of the world's poorest countries. When its HIV
infection rate crept past 20 per cent, many wondered how long the country
could last.
The
country's Minister of Agriculture said last year that production would have
been two or three times higher if not for the number of farmers who had
fallen ill or died. Zambia had full-scale food emergencies from 2002 to
2004, caused partly by lack of rain but hugely compounded by AIDS. The
disease has also gutted other industries as well -- the Zambia Business
Coalition says 82 per cent of known causes of employee deaths are
HIV-related. The health system is at 50 per cent of necessary staff levels;
Zambia has 600 of the 1,500 doctors called for in the national plan; only a
third of nursing jobs are filled. In ministry buildings, there are whole
hallways of empty offices, with staff sick, dead or at funerals.
And yet,
Zambia's economy grew by 5.2 per cent last year. Copper mines are reopening
as mineral prices push higher; the government is gearing up for a national
election; there are rush-hour traffic jams in the cities and a crowd turns
out for a public appearance by Miss Zambia 2006. Things are bad, but this is
not a failed state.
Paul
Spiegel, a Canadian in charge of AIDS policy for the UN High Commissioner
for Refugees and a veteran of work in hard-hit African states, says the
question increasingly puzzles researchers in all fields. "The hypotheses on
everything from . . . orphans to states collapsing due to lack of people
have not happened, and why is that? It's clear that coping strategies are
more resilient than anticipated, but we haven't done enough research at
community level to really know how it's working."
In Zambia,
it is clear that the basic resilience of communities -- the capacity to
absorb emotional, physical and financial burdens -- has proven far greater
than anyone would have dared predict.
"It's
amazing what this human race can do in the face of the most adverse
conditions," says Brian Chituwo, a doctor who is minister of both health and
education.
In most
cases, communities have stepped in to pick up the burden of care and support
that can't be met by the state. Take Stanley Chinoya from Kitwe, who spends
his mornings at an orphan centre run by a local community group, Children In
Distress. Here, he is finally learning his letters, and the volunteer
teacher hopes he can catch up to children his age in a year or two. The
group will then use international donor money to pay his school fees.
Another local charity recently arranged for Stanley to receive
anti-retroviral drugs.
Martin
Rupiya, an expert on AIDS and security with the Institute for Security
Studies in Pretoria, says the second thing to note about is that, in many
cases, the state's presence was slim to nil to begin with.
"There are
lots of parts of Africa where government simply doesn't exist," he says.
"The Western idea of the state doesn't recognize the lifting done by
traditional structures."
Catherine
Sozi, a Ugandan doctor who heads the UNAIDS mission in Zambia, says Zambians
organized to take care of the sick at home, to foster orphans, to pool their
labour, because there was not and never had been any sort of official
structure that might fill those roles. Indeed, she said, Zambia's national
response to AIDS has been predicated on the idea that community groups will
do the work.
"The
government can provide policy and they're not bad at that, but they're not
implementers, they can't do," she said.
Two other
factors have helped to stave off the anticipated disaster. First, there are
signs that HIV infection rates are levelling off or even dropping. Zimbabwe,
Kenya and Ethiopia have all, in their latest surveys, found indications of
slowing infection rates. And HIV, by its nature, allows time to adapt, with
a lag of up to 10 years from the time people get infected to the time they
begin to fall ill, and another few years before they die.
Most
important, though, is treatment. Although Africa lags woefully in the
provision of life-prolonging ARVs to people with HIV, it is also true that
treatment has accelerated beyond what many people imagined possible just a
few years ago.
Zambia, for
example, has 51,000 people on public treatment -- only a quarter of those
who need it, but up from 3,000 at the start of 2004. That number is enough
to start to cushion the impact of the disease; it's the reason why there is
only one person in each bed in Kitwe Central Hospital, and why there are men
available to work in the area's reopened copper mines.
Military
forces, meanwhile, have continued to function, even though their personnel
-- young men in environments where alcohol and commercial sex are widely
available -- are prime candidates for infection. Military discipline and
structure means that all personnel can be inculcated with prevention
messages, tested for HIV, treated and closely monitored. As a result, most
African militaries now far outdo their governments in responding to the
disease.
And despite
the undeniable losses of productive young workers, African economies have
not imploded as was anticipated -- partly because of the reality of who dies,
says Alan Whiteside, head of the Health Economics and HIV-AIDS Research
Division at the University of Kwa-Zulu Natal in South Africa.
"Some
people are more important for driving a political system, an economy, etc.,"
Prof. Whiteside muses. "And the reality is that if you in some way have your
drivers, your core, protected -- either because they are not infected or
they can access ARV therapy -- then the epidemic won't have the same effect.
I don't mean just the elite, you need the entrepreneurs . . . people who
make things happen."
That's why
Zambia is still showing modest growth, he says. It's why Uganda, the first
African country hit by AIDS, averaged 6.5-per-cent annual growth through the
past decade, becoming a development poster country even as deaths from the
disease hit their highest levels. It's why South Africa, the most infected
country in the world, posted its 87th consecutive month of growth in March.
The other
doomsday prediction that did not come true in Africa was that of the orphans.
Yes, the streets of Lusaka and Kitwe are filled with street children, a
sight almost unknown of 12 years ago. But they haven't organized into
criminal gangs and aren't considered an imminent threat to national security.
"I don't
think that gangsterism will ever materialize," says Father Michael Kelly, an
Irish Jesuit priest who has taught in Zambia since 1955 and is a leading
expert on orphans. "There are young men and women in the [slums] trying to
organize to do something -- it may be very shallow, but they are trying to
hold the fabric together."
But Father
Kelly and many others wonder how long it can last.
"Every
community response has a limit," Dr. Chituwo says. "And the family network
is cracking."
Dr. Sozi
from UNAIDS agrees. "We're underestimating the impact, still. Go to clinics,
go to the schools, if you're talking about development of a country --
that's where you're supposed to see it. Go to farms, the agricultural sector,
the towns outside the capital -- the infrastructure is collapsing. It's too
early to say disaster has been staved off."
Because of
the way AIDS works -- waves of infection, then waves of illness, then waves
of death -- it's possible only to say that total disaster has been delayed,
Prof. Whiteside notes.
"We are
still at the beginning of this . . . To really know what the epidemic means,
we will have to wait 35 years," he says.
Anne Mumbi,
the director of Children in Distress, watches Stanley Chinoya struggle with
his letters and says something else gets lost in the doomsday scenarios.
"Zambia
without AIDS would have been very different," she says. "We've lost quite a
lot of those brilliant young people that I knew at university . . . in terms
of human resources, well, your development depends on the human capacity you
have." Zambians have proved resilient, yes -- but at what cost?
"The
miracle of it is that somehow people survive," she said. "But you can't call
it living."
Resilient
states
In the late
1990s, as the world woke up to what AIDS was doing to Africa, experts began
making alarmed predictions about the worst-hit countries. But although the
damage has been great, these countries have not collapsed. Infection rates
are dropping, treatment has improved and economies have churned on, while
local communities have stepped in to take over many state roles.
Life expectancy
Average life
expectancy at birth (years)
| |
1980 |
2004 |
| Botswana |
61.84 |
35.49 |
| Central African
Rep. |
47.60 |
39.41 |
| Lesotho |
53.20 |
35.60 |
| Malawi |
44.86 |
40.22 |
| Mozambique |
42.77 |
41.83 |
| Namibia |
58.07 |
47.46 |
| South Africa |
57.13 |
44.64 |
| Swaziland |
51.58 |
42.21 |
| Zambia |
51.59 |
38.08 |
| Zimbabwe |
59.33 |
37.25 |
Population
Total population, in millions
| |
1980 |
2004 |
| Botswana |
1 |
1.8 |
| Central African
Rep. |
2.3 |
4 |
| Lesotho |
1.3 |
1.8 |
| Malawi |
6.2 |
12.6 |
| Mozambique |
12 |
19.4 |
| Namibia |
1 |
2 |
| South Africa |
27.6 |
45.5 |
| Swaziland |
0.6 |
1.1 |
| Zambia |
6.1 |
11.5 |
| Zimbabwe |
7.3 |
12.9 |
Gross domestic product
Per capita (U.S. dollars)
| |
1980 |
2004 |
| Botswana |
$1,077.48 |
$3,667.53 |
| Central African Rep. |
$313.57 |
$225.29 |
| Lesotho |
$309.65 |
$539.62 |
| Malawi |
$161.70 |
$152.98 |
| Mozambique |
$179.01 |
$274.93 |
| Namibia |
$2,028.89 |
$2,034.65 |
| South Africa |
$3,463.25 |
$3,312.22 |
| Swaziland |
$980.59 |
$1,356.96 |
| Zambia |
$450.51 |
$336.15 |
| Zimbabwe |
$598.68 |
$465.69 |
*constant 2000 U.S. dollars
SOURCE: THE WORLD BANK
The business of fighting
AIDS
AIDS is a direct threat to
the economic, social and political development and stability of many
nations on every continent except North America, says Richard Holbrooke
The XVI
International AIDS Conference beginn in Torontois by far the most
important of the many AIDS conferences that regularly take place around
the world. Let us hope it is a wake-up call that AIDS is more than the
worst health crisis in history -- although it is that-- it is also a
direct threat to the economic, social and political development and
stability of many nations on every continent except North America.
Some speakers at
the conference may talk of progress in specific areas of the war on AIDS
-- development of an effective microbicide that women can use to protect
themselves before sex, for example; or in the (far too) slow spread of
confidential testing and counselling. But let no one think we are winning
the war against HIV/AIDS. Every single year since the disease was first
identified a quarter of a century ago, the number of people who are
infected has grown, as has the death toll. The most that can be said is
that we are losing at a slightly slower rate. That is not progress, at
least not in my book.
You might think
that, by now, everyone knows this; after all, AIDS and Africa were the
main themes of Tony Blair's Group of Eight summit last year in Gleneagles,
Scotland, and the subject of the only United Nations Security Council
special sessions ever devoted to a health issue. But general awareness
travels slowly, and with all the other urgent business facing the leading
nations in the world today, many people still turn away, especially since
AIDS is spread largely through sexual contact, a subject that makes many
people and cultures uncomfortable.
But ignoring the problem will only make it worse. Governments that are in
denial are most likely to pay a far higher price. South Africa, with the
largest HIV prevalence in the world, would be in better shape if its
leadership, especially its health minister, were more candid, more
decisive and more aggressive. (Although the minister is a doctor, she
regularly gives speeches suggesting that olive oil and garlic can prevent
AIDS, and continues to give serious consideration to hare-brained theories
that the HIV virus does not lead to AIDS; her stand has confused many
Africans and weakened the prevention message greatly.)
The massive
effort required to stop this disease must be led by governments and
international organizations such as WHO, UNAIDS and the Global Fund to Fight
AIDS, Tuberculosis and Malaria. But, in many places, the governments are
simply not able to do the job because of limited resources or -- as in the
case of South Africa, Russia, Ukraine, most of the Caribbean and, until
recently, India and China -- because of denial.
The only
hope we have to start winning the war against AIDS is to have a clear and
consistent message to overcome stigma and dismantle denial.
At the same
time, we need to mobilize society for proven, effective interventions,
including widespread HIV testing so people who test negative can remain
negative, or be referred for treatment if they test positive; consensus on
the use of condoms to prevent the sexual spread of HIV; development and
distribution of anti-AIDS drugs that work well if appropriately prescribed
and adhered to; and rolling-out treatment programs in the developing world
is possible, feasible and often can be more effective than treatment in
industrialized countries.
To help
fill this gap, there is a huge potential role for the business sector. It
was this simple theory that led to the creation of the Global Business
Coalition on HIV/AIDS (GBC), a non-governmental organization that has grown
from fewer than 20 companies five years ago to more than 220 today.
These
companies, based around the world and employing more than 11 million people,
have committed themselves to a broad range of activities.
These vary
according to individual company core competencies but generally aim to
educate and test workers and spread information about AIDS to their local
communities or, in the case of great communications companies that are
members -- such as Viacom, HBO, Reuters, BBC World Service, Yahoo, STAR,
Sohu.com, Independent Newspapers, the French network TV5, and many others --
to a global audience. In some cases, GBC members offer treatment to infected
workers and often to their families (this group includes Anglo American, De
Beers, Eskom of South Africa, Coca-Cola, DaimlerChrysler, Heineken and
Lafarge). A few of our members, led by American Express and Gap, have gone a
step further and joined Product RED, a campaign committing a percentage of
sales from certain products, such as the American Express RED Card, to the
fight against AIDS. The GBC is especially proud of its eight Canadian
members, which include Alcan, Barrick Gold, Indigo Books and Music, M*A*C
Cosmetics, Power Corporation of Canada, Royal Bank of Canada, Sun Life
Financial and TD Bank Financial Group. These companies make corporate Canada
a leader in the effort to involve business in this fight.
Smaller
businesses cannot usually do much on their own, and here more government
effort is essential. And public calls, like those of Stephen Lewis, the UN
Secretary-General's special envoy for HIV/AIDS in Africa, that
private-sector corporations must devote a fixed 0.7% of pre-tax profits to
the AIDS effort are simple-minded and work against the very noble goals they
seek. But we should not argue over such empty rhetoric; there is work to be
done. At the end of the day, when our careers -- in whatever field we have
chosen -- are over and our children and grandchildren ask us what each of us
did to fight the worst health crisis in history, what will our answers be?
Will we have any answers at all?
Richard
Holbrooke, a former U.S. ambassador to the United Nations, is president of
the Global Business Coalition on HIV/AIDS.
Here's what politicians
should understand about HIV/AIDS
There are moments in history when it seems both especially difficult and
particularly offensive to try to weigh one collective human tragedy
against another. But if the hierarchy of human catastrophe can, at the
very least, be determined in lives lost day in and day out, then the HIV
epidemic still ranks at the top of this era's list.
HIV/AIDS continues
to kill more than 5,000 people each day -- a body count far higher than
the number of individuals who have died in recent military conflicts
anywhere in the world and also higher than the number of deaths
attributable to any natural disaster in recent memory. Yet, HIV/AIDS no
longer receives the attention it once did. It is almost as if this
epidemic has been with us for so long that we have become immune to it.
HIV can be
prevented. The XVI International AIDS Conference, which begins on Sunday
in Toronto, will unfold in an atmosphere of magnified worldwide attention
to the myriad issues surrounding AIDS, but with fewer politicians in the
crowd to hear the message than there should be, and they're the ones who
need to listen.
Notwithstanding the recent infusion of funds by the Gates Foundation
toward the goal of a safe and effective HIV vaccine, a solution that
radical is still years away. But there are measures that can be
implemented almost immediately to deter HIV transmission:
Politicians
should understand that religious values will not prevent millions of people
who profess to adhere to those values from having unprotected,
non-monogamous sex. The promotion of condom use should not replaced by
alternatives that hinge on breathtaking transformations in human nature.
Condom use can prevent the spread of HIV, period.
Politicians
should understand that the establishment of safe needle-exchange programs
for intravenous drug abusers will not promote illicit drug abuse but will
help to prevent the spread of HIV. Promotion of these programs should not be
a matter of political debate, since their implementation will neither
promote promiscuous sex nor illicit drug use for children of parents who
impart their own family values to their offspring.
A less
politically charged prevention tool has emerged with evidence that male
circumcision in poor countries may help to reduce the spread of HIV. (Circumcision
is thought to interfere with transmission because the foreskin contains
cells that are important portals of entry for HIV into the body.) World
health officials are now assessing how best to train surgical specialists to
perform circumcisions in areas where the procedure is not widely available.
Politicians should understand the importance of financing this training.
We also
need to promote prevention research. One key initiative is the development
of microbicide products that women can self-administer intra-vaginally
before sexual relations to protect themselves against HIV. Many women,
particularly in developing countries, understand that their sexual partners
put them at risk of HIV infection and that condoms represent an effective
barrier but are not empowered enough to insist that a condom be used. The
study of antiviral vaginal gels and foams is now far advanced, but
additional resources are urgently needed to fund the testing of these agents.
And we need
further study on pre-exposure prophylaxis of HIV disease. This concept is
based on the notion that the same antiretroviral drugs used to treat people
after infection might also interfere with the initial HIV infection, if
taken daily by individuals at high risk. Sadly, clinical studies that were
to have tested this hypothesis in developing countries have now been stopped,
in part because of pressure by those who thought they were being performed
to benefit the drug companies that provided their drugs for testing. The
likely consequence of success in clinical trials would be that such drugs
would be manufactured at low cost by generic manufacturers.
These
issues all fall at the intersection of clinical science, public health
policy, and the ethical considerations that must guide research and clinical
trial implementation. Given the status of HIV as our common enemy in the
most important war that humankind is now fighting, let's hope the political
will to translate scientific achievement into successful prevention efforts
will prevail.
Dr. Mark
Wainberg is director of the McGill University AIDS Centre and co-chair of
the XVI International Conference on AIDS.
Million receiving ARVs in Africa
More than
one million HIV-positive people are receiving anti-retroviral therapy in
sub-Saharan Africa, a UN agency says.
The World
Health Organization says there has been ten-fold increase in treatment since
December 2003.
The UN's
goal is to provide universal access to HIV prevention programmes, treatment,
care and support by 2010.
WHO
HIV/Aids Director Dr Kevin De Cock told Aids conference delegates in Canada
much still needed to be done.
Although
sub-Saharan Africa has the greatest number of people on treatment, and the
second-highest rate of treatment coverage among those who need it, the
region still accounts for 70% of the global unmet treatment need, Dr De Cock
said.
"We have
reached just one-quarter of the people in need in low and middle-income
countries, and the number of those who need treatment will continue to grow,"
he said.
"Our
efforts to overcome the obstacles to treatment access must grow even faster."
Some 24% of
people needing ARV treatment worldwide were receiving it by June 2006, he
added.
Fruit and drugs on SA HIV
display
Lemons and
garlic are displayed next to condoms and anti-retroviral drugs on the South
African stand at Toronto's international Aids conference.
Apples,
nectarines and other tastier fruit were apparently included earlier, but
were soon eaten, an official said.
South
Africa's health minister has long promoted a diet including garlic and lemon
as a way of treating Aids.
In 2004 the
government began providing Aids drugs but activists still question its
commitment to fighting HIV.
The
exhibition represents "South Africa's response to Aids - the most
comprehensive in the world," an official at the stand told the BBC's Lee
Carter.
"The theme
is talking about issues around nutrition, and also prophylaxis and
treatment," he added.
But the
approach attracted controversy, particularly since the bottles of
anti-retroviral drugs were only added to the stand some time after the fruit
and vegetables went on display.
'Despicable'
One doctor
from the paediatric Aids unit at Baragwanath Hospital in Soweto challenged
the organisers of the exhibit to provide scientific evidence that any of the
foodstuffs on display were clinically effective.
"It's
despicable that you bow to the minister's wishes and put the exhibit
together in such a way," Dr Harry Moultrie said, quoted by Beeld newspaper.
At the same
time, a Southern African Development Community (SADC) report says the main
reason for the spread of HIV/Aids is people who have multiple sexual
partners and are not consistently using condoms.
The study
says casual sex and intercourse with sex workers are no longer the main
causes of new HIV infections.
It says
traditional high-risk groups, such as prostitutes, mineworkers and truck
drivers, are, in fact, better protecting themselves against infection.
The orphan epidemic -
Aug. 17, 2006
Kerrel McKay was
just nine years old when her father was diagnosed with HIV.
She didn't really
understand what it was, but figured it must be bad. After all,
neighbours and relatives refused to go near him, money began to
dry up because of his health-care costs and he was slowly
wasting away from a disease he refused to speak about.
She had no one to
turn to and the fallout was shattering.
"I was suicidal, I
thought about it every day," recalled McKay, a 21-year-old AIDS
activist from Kingston, Jamaica and one of 26,509 people at the
International AIDS Conference in Toronto.
"I just thought
that if I were dead then I wouldn't have to face it. I was
watching him die and not even able to speak with him about
HIV/AIDS."
She's lucky to
have met someone who inspired her to channel her heartache into
helping others in similar predicaments.
Today she runs
AIDS prevention outreach programs for Jamaica's health ministry,
a job that often takes her into communities where she meets
children who, like her, lost one or both parents.
The
socio-psychological impacts on children orphaned by AIDS are
immense, said McKay, who watched her father die when she was
just 15.
But they're issues
that are rarely addressed and aren't being properly highlighted
at the conference.
There have been
numerous sessions on issues such as prevention of
mother-to-child transmission of the virus that causes AIDS and
pediatric treatment, but there hasn't been enough talk about the
traumatic stress endured by children around the world, said
Brenda Yamba of Save the Children Mozambique.
"When you look at
the issues that affect orphans and vulnerable children, you're
dealing with an entire lifetime," said Yamba, who has also
worked with children in Zambia and Malawi. "Every (facet) of
their lives is affected."
And the number of
affected children is on the rise, so it's an issue that demands
serious attention.
According to a
report released this week by UNICEF, there are about 15 million
children orphaned by AIDS, 12 million of whom live in
sub-Saharan Africa. By 2010, it's estimated that number — which
includes children who have lost one or both parents — will grow
to at least 18 million.
This
is an epidemic of orphaning the likes of which we've never seen before,"
said Doug Webb, children and AIDS adviser for UNICEF eastern and
southern Africa. "Even if the number of infections stopped tomorrow,
the number of orphans will continue to go up."
And
while the figures are startling, he said there are countless children
in living in homes where there is a parent or caregiver dying of AIDS.
Essentially, there are millions more in the queue waiting to become
orphans.
And
the health implications are devastating, he said. Orphaned and
vulnerable children are at a higher risk of dropping out of school,
suffering malnutrition and experiencing depression. And substandard
education puts them at higher risk of HIV infection, especially
adolescent girls and young men in the 15 to 24 age group.
The
long-term impact of AIDS on children is not known, in part because the
world has never experienced an epidemic of this kind.
"We've
got a lot of children who will watch their parents die," says Webb,
adding the grief and emotional separation they experience will make
them more susceptible to suffering depressive disorders, mental
illness and ill health as adults.
And
the future impact on society is frightening, particularly for a
continent where virtually everyone has been affected in some way by
AIDS, he said.
"We're
seeing numbers of orphans that are eight to 10 times higher than they
were pre-AIDS," he said. "And we don't know what that means to the
societal level and what the tipping point is.
"We're
not looking at that effectively — we're focusing on trying to reach
the children with immediate services."
For
now, reaching out to those children is something Goldmark
Owoola-Adeojo does in her hometown of Lagos, Nigeria.
The
11-year-old AIDS activist strives to give a voice to children affected
by AIDS and address their issues and concerns through her organization,
Live Alive Foundation.
When
she isn't busy speaking out on the scourge of AIDS — be it at a
conference or a bus stop — she often visits with children who are
either living with the disease or have been orphaned by it.
"Whenever
my mother buys extra food stuff I cook it and take it to the children
and will sit and listen to them," said Goldmark, whose activism was
inspired by her mother, a journalist and HIV/AIDS educator.
They
tell harsh tales of being stigmatized, failing school, being forced to
work and relatives who don't want to care for them. The heartbreaking
stories are difficult to hear, said Goldmark, the youngest delegate at
the Toronto conference. It fuels her resolve to make their stories
known and voices heard.
"It
is important we listen to them," Goldmark said, adding she's "passionate"
about fighting on behalf of those who cannot fight for themselves.
AIDS immunity under the
microscope - 17/08/06
One in
every 300 people living with HIV never becomes sick or needs to take even a
single drug to fight their infections, according to a surprising statistic
released at the International AIDS Conference on Wednesday.
Researchers
have long known that some people have a natural resistance to the AIDS
virus. But only now, 25 years into the epidemic, are they discovering the
scope of a phenomenon they're calling “elite controllers.”
These are
people with HIV who have the mysterious ability to stop the virus from
replicating, even without medications. An international research consortium
is now anxiously recruiting elite controllers for a new genetics study.
“If we
could discover how these individuals can co-exist with this virus without
damage to their immune system and could find a way to replicate that ability
in others, we would have a recipe for halting the HIV epidemic,” said Bruce
Walker, a professor at Harvard Medical School and one of the study's key
organizers.
Researchers
believe solving the biological mystery could form the basis of a vaccine.
“There is a
reasonable chance we will come up with something very important with this,”
said Dr. Walker. “We need patients.... We need to get the word out.”
Researchers
have to enroll at least 1,000 elite controllers in order to make sure they
have enough numbers to make meaningful genetic discoveries. About 200
patients are expected to be recruited from Canada, where 25 patients have
already signed on.
Rafick-Pierre Sékaly, a McGill University immunologist and study
investigator, said the Canadian subjects have been HIV positive for seven to
15 years but are healthy and have never required treatment.
In most
people infected with HIV, the human immune system cannot stop the virus from
replicating without medication. In the absence of treatment, HIV makes so
many copies of itself it eventually overwhelms the host's immune cells and
the person grows sicker.
But an
elite controller has fewer than 50 copies of HIV per millilitre of blood,
Dr. Sékaly said. This is a level considered undetectable by current tests.
Researchers also hope to recruit 1,000 so-called ‘viremic controllers.'
These are healthy people whose blood samples show 2,000 viral copies or less.
The
researchers had stipulated at the outset that subjects had to be infected
for at least a year to qualify for study enrolment. But doctors have found
the 200 patients enrolled so far have lived sickness- and treatment-free
with HIV for an average of 15 years.
“You're
sitting across from these patients,” said Dr. Walker, “and you just feel
like, oh, the answer is there right in front of you, we've just got to fish
it out of them.”
He also
guessed it was unlikely that these people would ever see their infections
progress, and that they would, in the end, likely die of something other
than AIDS.
Loreen
Willenberg, a 52-year-old landscape designer from Diamond Springs,
California, learned in 1992 that she was HIV positive. Since then she has
battled the emotional impact associated with the stigma of having HIV in a
small town, and opted only to “come out” with her HIV status earlier this
year.
But the
disease, she said, took no physical toll: “I'm in perfect health,” Ms.
Willenberg told a press conference Wednesday. “I've maybe had one cold in 14
years.”
In response
to a journalist's question about her diet, Ms. Willenberg said she eats many
fruits and vegetables, but that she is not a vegetarian. She added that she
is not a fast food eater and never has pop or candy in the house.
But Dr.
Walker noted other elite controllers in the study eat fast food “non-stop.”
The test
subjects also do not have in common any of the genetic traits known to be
associated with HIV resistance, said Dr. Walker, who is also director of the
Partners AIDS Research Center at Massachusetts General Hospital.
Neither
have these elite controllers “contracted some wimpy form of this virus,” Dr.
Walker said. Some of these protected patients know who infected them and
those people have gone on to get ill. But researchers still plan to sequence
the DNA of the viruses infecting them.
It is
unknown at this point if any elite controllers have ever passed on HIV. But
having a low viral load is believed to significantly reduce the chance of
transmission.
Doctors
have long remarked on the puzzle of the patients, also known as “long-term
non progressors.” But it wasn't until the mid-1990s when viral-load testing
became available that researchers were able to clearly identify people who
could keep HIV in check.
Dr. Walker
said that a majority of these elite controllers have not disclosed that they
are HIV positive.
“They also
feel a sense of guilt because they are survivors,” Dr. Sékaly said. “They
have seen their friends die and they have never even been sick.”
Ms.
Willenberg once wrote an article on her strange condition, entitled,
“Partially HIV Positive.” “She didn't feel like she belonged to the infected
or the uninfected,” said Dr. Walker.
Dr. Walker
estimates that 2,000 people in North America are elite controllers. But he
suspects the one-in-300 number applies to HIV infected people all over the
world. Research in South Africa, he said, indicated a similar finding.
Just
recently, Dr. Walker said, he gave a course to 500 doctors who treat AIDS
patients and asked how many had elite controllers in their practice. “Half
the hands in the room went up,” he said. “Then I asked, “what have you done
with [them or this information] and they throw their hands up in the air ...
no one knows.”
Among the
theories researchers are considering is that elite controllers may have
natural anti-viral factors in their cells. It could be that the immune
system of the elite controllers offers up a weaker immune response to HIV,
preventing the body from over-killing its own T-cells. But all of these
things are likely to be effected by genetic traits.
The study
team plans to take blood and DNA from study participants and promises strict
confidentiality.
Their
genomes will be scanned for mutations already identified in the Haplotype
Map. That map spun off the human genome project and pinpointed the most
common gene mutations in four different ethnic populations. The McGill team
will then analyze the function of the important traits they find.
“One of the
key problems with the development of a vaccine,” said Dr. Sekaly, “is that
we don't know what response to mimic."
Drug access is critical,
activists warn
TORONTO
— Critical issues of access to life-saving medications are being overlooked
in the excitement about new technologies and prevention methods, activists
warned at the international AIDS conference yesterday, with the risk that
the hundreds of thousands of people newly started on anti-retroviral drugs
in poor countries could be left without medications in a year or two.
The price
of the so-called “first line” of drugs — the optimal initial regimen for a
person with AIDS — has come down to $132 (U.S.) per patient per year, thanks
to competition from generic companies and activist pressure. But within
three or four years, people taking those drugs become resistant, and need to
switch to a new regimen — which today costs at least six times more.
This is
costly for a country such as Canada, but unsustainable for one such as
Malawi, which is already using the bulk of its health budget to put people
on first-line drugs.
The problem
looms increasingly large as the world's poorest countries, which are also
some of the most infected, scramble to get people on to anti-retrovirals.
On Tuesday,
former U.S. president Bill Clinton said one of the key lessons at the
conference for him was the urgent need for these drugs and the fact that
their existing prices put them out of reach for most developing countries.
Today the
standard second line of treatment in Africa costs $1,500.
“That's 10
times the price of the first line, so if 10 per cent of your patients go on
it, your overall costs double,” said Anil Soni, director of pharmaceutical
services for the Clinton HIV/AIDS Initiative. “So the first issue is that
the products are not available and patients are dying today.
“But the
macro issue is that this is driving an exponential increase in cost, just as
we're talking about universal access.”
And it isn't
just “second line.” The World Health Organization released recommendations
this week on optimal AIDS treatment, but the new list of drugs includes many
that are priced far out of reach for developing countries.
The newly
recommended first line, for example, is a combination with Tenofovir, which
is not available in many developing nations. “It means countries can't
implement the guidelines,” said Alexandra Calmy, HIV-AIDS adviser for the
access to essential medicines campaign.
Compared
with the current first line used all over Africa, the combination with
Tenofovir causes fewer of the side-effects that plague people on ARVs, such
as nerve damage and disfiguring fat redistribution.
Much of
this debate centres on the drug Kaletra, a key component of second-line
treatment. Abbott Laboratories introduced a new version of the drug that
doesn't require refrigeration — essential for African countries. But Abbott
is not giving a voluntary licence to any generic company to make the drug (spokeswoman
Jennifer Smoter said the manufacture of the drug involved proprietary
technology), insisting instead that it will scale up production to make
quantities for the developing world.
And new
pricing announced on Monday did little to placate organizations of people
with AIDS desperate for the drug. In Thailand, for example, Abbott will sell
the new Kaletra for $2,200 per patient per year — down from $3,000.
But in a
country where the monthly wage of a university-educated office worker is
$120, it is still not feasible, said Nathan Ford, who has been struggling to
get the new Kaletra for Thai AIDS patients treated by Médecins sans
frontières (Doctors Without Borders).
Meanwhile,
those working in front-line HIV health services in Canada said yesterday
that people at the conference may be left with the “false impression” that
everything in this country is fine.
“It's a
total myth that people have access or equal access to drugs in Canada,” said
Louise Binder, the chair of the Canadian Treatment Action Council, which
lobbies on behalf of people with HIV.
Bigger,
wealthier provinces such as Ontario, Quebec and Alberta tend to pay for and
provide HIV drugs. But not the Maritimes, she said. “People literally have
to move to stay alive,” she said.
As well,
Ms. Binder said there are about 19 different federal drug plans that cover
HIV medications. Some drugs that aren't covered for aboriginals are covered
for military personnel or pensioners, she said.
Delivering vital medical care —
on the house
TORONTO
— Some came requesting rapid HIV tests. Others sought methadone for their
opiate addiction. And a fair number, looking tired and weary, came with more
mundane complaints of sore throats and headaches.
More than
300 people attending the International AIDS Conference during the past few
days have sought medical care at the health clinic, a cheerful place tucked
in a basement corner of the Metro Toronto Convention Centre.
At the side
of the clinic, which usually functions as a bar, are all the usual things
one might expect in a makeshift supply cabinet and a little more:
antibiotics, anti-inflammatory drugs, medicines to treat sexually
transmitted diseases, pregnancy tests and Plan B, an emergency contraceptive.
“The idea
of providing health services is to make it convenient and cheap,” said Brian
Cornelson, the conference's medical director. “What we want people to do is
minimize the time that they would need to be away from the conference to get
health care and not to be avoiding health care at the early stage of an
illness because they are afraid of the cost and uncertainty.”
At the free
clinic, doctors and nurses see those with addictions, patients suffering
from headaches or fatigue, and they see the unusual — such as a man who had
a malfunctioning screw on his leg brace.
Wamarou
Traore, a 49-year-old virologist from Burkina Faso, a West African country,
was fiddling with his custom leg brace, a device made necessary after he was
struck by polio as a child.
“It's all
this walking around,” Dr. Traore said in an interview, in explaining how the
screw was about to break.
Dr.
Cornelson, an amiable man with a towering stature, examined his patient's
brace and recognized it had to be fixed straight away. And he managed to
work a little bit of magic: He telephoned St. Michael's Hospital, where one
of his contacts arranged for Dr. Traore to get the brace fixed free of
charge at an orthopedic appliance provider on the east side of Toronto.
No sooner
did that end when Mark Bardsley, a 46-year-old from Philadelphia, came in
complaining of dizziness, a tingling from head to toe and difficulty
concentrating. The night before, he said, he suffered from a headache but
nothing as severe as the migraines he had in the past.
Mr.
Bardsley, who is also a registered nurse, gave his history: he has high
blood pressure, is HIV-positive and has suffered some recent prostate
problems. More than a decade ago, he suffered a transient ischemic attack,
known commonly as a mini-stroke, following a visit with a chiropractor.
After doing
a neurological exam and checking and rechecking his blood pressure, Dr.
Cornelson, who works at St. Michael's Hospital as an HIV primary care
physician, was concerned that Mr. Bardsley may be having another mini-stroke.
But after a
careful examination, he was satisfied Mr. Bardsley's condition was likely
related to his elevated blood pressure and the aftereffects of a migraine.
He instructed Mr. Bardsley to increase his blood pressure medication and, if
his condition worsened, he should call 911 and go to hospital.
The
assurance that HIV test results in Canada are kept confidential was part of
the draw for five patients seeking to know their status. Rapid test results
of the five — three from Africa, one from Iran and one from Canada — were
all negative, Dr. Cornelson said.
As well,
seven patients have received methadone for their opiate additions, either by
prearranging care before coming to Canada for the conference, or in a few
cases, requiring it after it was spilled or lost. While the services of
health care staff are free, the methadone, which is given orally with an
orange drink, is not. The patient must pay.
“Some have
come once and some have come on more than one occasion,” said Thea Weisdorf,
a family physician at St. Michael's who is on call to treat those who
require methadone. “Some missed seeing their regular provider or may have
gone a few days without methadone.”
Whatever
brings patients to this health clinic, many of them will be greeted by a
smiling Grace Bezaliel, who works at the front desk of the clinic as a
clerical administrator. She took a week's vacation from St. Michael's so she
could work for free in the clinic during the conference.
“I came
here as a refugee from Zimbabwe in May of 2002 and I want to give something
back,” Ms. Bezaliel explained. “I have lost friends to AIDS.”
Playing up the ‘play safe'
message
TORONTO
— Every day, an estimated 1,500 children under the age of 15 become infected
with HIV/AIDS. A larger number still lose one or both of their parents to
the disease, further swelling the ranks of the 15 million AIDS orphans.
Getting to
those children — the next generation — with a strong prevention message is
seen as one of the key elements in reining in the epidemic.
But how,
especially when far too many children, and girls in particular, do not have
access to education?
“Sport,
physical activity and play are low-cost, effective tools to reach young
people with key prevention methods about HIV/AIDS,” said Bruce Kidd, dean of
physical education at the University of Toronto. He has done extensive work
in Zambia
Thursday,
the 16th International AIDS conference will feature the first session on
sport as a tool for HIV/AIDS education.
Right to
Play, a Toronto-based humanitarian group founded by Norwegian speed-skating
star Johann Olav Koss, uses sport and play as development tools for children
in 23 of the world's poorest, war-ravaged countries. It reaches an estimated
500,000 children a week.
The “Live
Safe, Play Safe” program focuses specifically on HIV/AIDS education. It's a
soft-sell approach, where the focus is on having fun, but education messages
are blended into the games children play.
For example,
“condom tag” involves designating one child as HIV/AIDS who tries to tag
others; the catch is that children carrying a condom balloon are safe. The
games are preceded by a discussion led by a coach-educator.
Safari
Kayisire, a Right to Play athlete-ambassador in Rwanda, said the key part of
the program is for children who have suffered through war, displacement and
the AIDS epidemic to have fun. But he added that, while shy at first,
children look to him as a mentor allowing him to have frank and open
discussions about HIV/AIDS.
“There's a
lot of misconceptions about AIDS, and it's tough for parents to talk to
their children about the problem,” Mr. Kayisire said.
Dr. Kidd
said children the world over love to play and fascination with sport and
games can be harnessed to teach them about HIV/AIDS. He said playing sports
builds self esteem and helps develop important social skills that are
essential as a child matures into a sexual being.
He cited
research that showed teenagers involved in sports initiate first intercourse
at a later age, have lower rates of sexually transmitted infections, lower
rates of teen unwanted pregnancy and are less likely to be victims of sexual
abuse.
Critics,
however, say it's a stretch to think this research, conducted in wealthy
countries, necessarily applies to children dealing with the harsh realities
of HIV/AIDS in developing countries. They also complain that the impact of
play-based programs has not been rigorously tested, and say money would be
better spent on more tried-and-true measures.
Joey Cheek,
a U.S. speed skater and Olympic medalist, made headlines around the world
when he donated the $40,000 bonus he received for winning gold in Turin to
Right to Play. He said he had no doubt about the effectiveness of the
program because he has seen the faces of children involved in the programs.
“This
really drives home the prevention message, and it does so in an intuitive
and fun way,” he said.
Canadian
speed skater Clara Hughes celebrated her gold-medal victory in a similar
fashion, donating $10,000 of her own money to Right to Play. That, in turn,
generated hundreds of thousands of dollars in donations from the public.
Mr. Cheek
has now travelled to the AIDS Conference to promote the group's latest
initiative. “I've spent my whole life in the selfish pursuit of Olympic
glory and I wanted to do something more meaningful,” he said
Thursday, Mr. Cheek and Mr. Kayisire will conduct a “Live
Safe Play Safe” session in downtown Toronto.
Chinese prostitutes raise AIDS
risk
Mainland
Chinese prostitutes, who flock to Hong Kong in large numbers to make a
living, are failing to protect themselves, and the number of HIV/AIDS
infections is expected to rise, social workers say.
Groups that
counsel sex workers say prostitutes are frequently questioned by police,
searched, detained and expelled if condoms are found on them. This is
prompting many prostitutes from mainland China to ditch the prophylactics
for fear that they will be caught.
Although
condoms are legal and Hong Kong laws do not empower police to detain anyone
found with a condom, police are intimidating and expelling prostitutes from
China, the groups say. Prostitution is legal in Hong Kong, but foreigners
violate the conditions of their stay if they are caught working.
Social
workers say such police must stop this practice or it will fuel a rise in
sexually transmitted diseases such as AIDS.
"Police
must stop using condoms as an excuse to arrest women because this makes
women vulnerable to disease," said Elaine Lam of Ziteng, the most
established help group in Hong Kong that is devoted to commercial sex
workers.
Loretta
Wong of AIDS Concern, another Hong Kong group, added: "The government is
contradicting itself. Although the Health Department is promoting condom use,
the police (are) using it to prosecute sex workers."
Their call
strikes a chord with key messages delivered at the 16th International AIDS
Conference this week in Toronto. Experts agree that preventing transmission
of the disease among prostitutes is crucial to controlling the AIDS pandemic.
"There are
still far too many instances where punitive laws, stigma, gender inequities
and lack of access to needed prevention and care services conspire to fuel
the HIV pandemic," said conference Co-Chair Dr. Mark Wainberg, director of
the McGill University AIDS Center
At the
conference opening on Sunday, Microsoft founder Bill Gates, whose foundation
has given hundreds of millions of dollars to fight AIDS, criticized
governments and politicians who refuse to talk to and help prostitutes.
"We need
tools that will allow women to protect themselves. This is true whether the
woman is a faithful married mother of small children, or a sex worker trying
to scrape out a living in a slum. No matter where she lives, who she is, or
what she does a woman should never need her partner's permission to save her
own life," Gates said.
POVERTY
Some
650,000 people in mainland China are living with HIV/AIDS, according to the
latest UNAIDS report, but only 32,500 are classified as female sex workers
-- a figure that social workers say is a gross underestimation.
In Hong
Kong, there are an estimated 300,000 prostitutes at any given time, half of
whom are from mainland China, Ziteng said. This figure stood at 200,000 in
1991.
Since Hong
Kong was returned to Chinese control in 1997, it has become increasingly
easy for mainland Chinese to visit the city, and many flock here for higher
wages, although they come illegally.
According
to Lam, prostitutes in China earn as little as five yuan (US$0.60) in
construction sites and along truckers' routes, to 300 yuan ($38) in posh
karaoke bars for the very few lucky ones.
Many choose
to come to Hong Kong, where they earn between HK$40 (US$5) and HK$150
(US$19) from each customer. They need to fork out, or borrow, at least 5,000
yuan (US$626) to secure two-way visas to Hong Kong, which are good for only
seven days.
"Because
they have such a short time to try to make money, many of the girls are
desperate and have no bargaining power. When customers offer to pay more for
unprotected sex, the girls will agree," said Chung Sze-wan of Ziteng.
Many women
are also ignorant. "We know of girls who have never seen condoms in their
lives," Chung said, adding that women who manage to recoup the money they
paid to come to Hong Kong and make a profit are those who do not insist on
safe sex.
"Many of
them have children and husbands and they want to protect themselves, but
they still take the risk. They literally ... risk their lives," she said.
Ziteng
provides free health screenings for sex workers and in a 2005 survey, seven
out of 58 women tested positive for the human papillomavirus, which is
sexually transmitted. There are more than 100 strains of this virus and
high-risk types can lead to cancer. Six of the seven women were mainland
Chinese.
The health
risk is not confined to China and Hong Kong as many of these Chinese women
are traveling further afield.
"We see
them going everywhere after transiting in Hong Kong. Malaysia, Singapore,
Italy, Japan, Australia, Taiwan," said Lam.
"People see
them as a carrier of the (HIV) virus but they are really victims because
they are forced not to use condoms."
'Elite' HIV patients mystify,
intrigue doctors
TORONTO - As many as one in 300 HIV patients never get sick and never suffer damage to
their immune systems and AIDS experts said on Wednesday they want to know
why.
Most have
gone unnoticed by the top researchers, because they are well, do not need
treatment and do not want attention, said Dr. Bruce Walker of Harvard
Medical School.
But Walker
and colleagues want to study these so-called "elite" patients in the hope
that their cases can help in the search for a vaccine or treatments.
"What in
the heck is going on in people that successfully control this virus?" Walker
asked a news conference held at the 16th International Conference on AIDS.
"If we can
figure out how people are doing that, we can try to replicate it."
So far
Walker and colleagues have not been able to find out why certain people can
live for 15 years and longer with the virus and never get ill. The AIDS
virus usually kills patients within two years if they are not treated.
Some even
appear to have weak immune responses, he noted. "Is it just that these
people got infected with a wimpy virus? The answer to that is no," Walker
said.
"Some of
the people know who infected them," he added, and in those cases, the person
who infected the "elite" patients always went on to become ill.
A few years
into the AIDS epidemic, researchers identified people who were called "long-term
non-progressors." These were patients infected with HIV who did not become
ill.
Many have
become ill as the years have gone by, and required treatment.
Walker said
a few of the long-term non-progressors were now classified as "elite"
patients. But the difference is that the "elite" status is clearly defined
by how much virus they have circulating in their blood.
Loreen
Willenberg, of Diamond Springs, California, is a newly designated "elite."
Now 52 and healthy, she said she became infected in 1992.
BAD DREAM
"I dreamed
that I was HIV positive," Willenberg told the news conference.
"I was
really going through a very bad flu." She sought testing, and after getting
an inconclusive result was later declared HIV positive.
HIV
patients are not immediately put onto drugs that can keep them healthy, but
wait until the virus reaches a certain level in the blood or until the virus
kills a certain number of immune system cells called CD4 T-cells.
Willenberg,
a landscape designer, never got to that point
"I am in
perfect health. I think I have had maybe only one cold in the past 14 years,"
she said.
Walker has
tracked down 200 elite patients and has now joined up with other prominent
AIDS researchers to find at least 1,000 "elites" in North America and as
many as possible globally.
Based on
research done so far, Walker estimates there are 2,000 of them in the United
States.
His team
wants to take blood and DNA samples to see what might be different about
them. Confidentiality is promised.
The
recently published map of the human genome will make this possible.
They will
compare key genetic sequences of the "elite" patients to genetic readouts
from healthy people and from other HIV patients. Maybe a few genetic
variations can explain what is happening, Walker hopes.
World Bank urges
Thai model for AIDS prevention
TORONTO -
Developing countries with few resources to fight AIDS could take their lead
from Thailand's prevention programs of recent years, which have allowed it
to provide nearly free drug treatments to patients, the World Bank said in a
report on Wednesday.
A former
hot spot for the virus, Thailand has more than halved the number of new HIV
infections over the past decade, and has won praise for its National Access
to Antiretroviral Programme for People Living with HIV/AIDS (NAPHA). The
program, started last October, provides antiretroviral drug treatment for
nearly 80,000 Thais, more than 90 percent of those who need it.
But the
seeds were planted about a decade earlier when Thailand made AIDS prevention
a top priority. It introduced initiatives such as the 100-percent Condom
Program, which promoted usage among sex workers.
This and
other programs, combined with a wide network of district level hospitals and
rural health clinics, have enabled it to control infection levels and
allowed it to implement the NAPHA program, the bank said.
Without the
prevention campaigns, Thailand would have had 7.7 million HIV cases and
850,000 AIDS cases in 2005, about 14 times more than today, the bank
estimated in a report during the 16th International AIDS conference in
Toronto.
"What we
figured is that for every dollar they spent on prevention, they saved about
$43 in treatment costs. That makes a benefit-cost ratio of 43-to-1, which is
unheard of," Mead Over, a World Bank economist and co-author of the report,
told Reuters.
The bank
estimates Thailand has avoided the need to spend an extra $18.6 billion on
treatment over the decade through 2012.
It says
countries such as China and India, where the epidemic is at an earlier
stage, could take lessons from the Thai programs
"Thailand's
past success with prevention is the most important reason the country can
afford universal access to (AIDS treatments) today. Furthermore it is an
essential condition of its continued ability to afford treatment in the
future," said Over.
UP TO 6 MILLION
COULD BENEFIT
Under the
NAPHA program, a patient can walk into a hospital or rural clinic and pay 30
baht (80 U.S. cents) for treatment.
In the
report, the bank says that 5 million or 6 million people worldwide could
immediately benefit from similar treatment, but only 700,000 are receiving
the therapy.
However,
the bank warns that Thailand's costs will rise as an increasing number of
surviving patients -- the bank estimates 572,500 Thais were living with
HIV/AIDS in 2004 -- turn to so-called second-line drugs, which are seven to
28 times more expensive than those given as the first course of treatment.
Many of
these drugs are patented and sold by large pharmaceutical firms. This means
Thailand will have to decide whether to pay their prices, negotiate more
favorable terms or exercise its rights under World Trade Organization rules
to issue compulsory licenses, which allow other makers to produce a patented
drug without permission from a foreign patent owner.
The bank
says by exercising compulsory licensing, Thailand could save about $3.2
billion in health costs through 2015.
But by
doing so, the government would run afoul of U.S. policy, which is a serious
concern, Over said, noting that $3.2 billion represents just a fraction of
the value of Thai exports to the United States in the past year.
MSF demands action for half
a million AIDS infants
TORONTO -
Urgent action is needed to treat more than half a million children in need
of AIDS drugs and to slash the price of these life-saving treatments, a top
medical relief agency warned Tuesday.
Doctors
Without Borders (Medecins Sans Frontieres, MSF), said at the world AIDS
conference here that only five percent of 660,000 children around the world
who desperately need antiretrovirals -- the so-called "cocktail" of AIDS
drugs -- had access to them.
The Nobel
Peace Prize-winning agency also lashed giant pharmaceutical firms for
failing to invest in pediatric AIDS drugs. Most child victims of AIDS live
in developing countries, and caring for them does little to swell corporate
profits, it charged.
Many infant
AIDS victims live in crushing poverty and contracted the disease as infants
from HIV positive mothers who themselves have no treatment or prenatal care,
MSF said.
Tragically,
without medical care, half the children born with HIV die before the age of
two.
"We
know that treating children works, but with better tools, we could be
treating so many more," said Moses Masaquoi, a doctor with MSF in
Malawi.
"We see the
number of children born with HIV constantly growing in Africa, because
expecting mothers don't have access to ante-natal care and children born to
HIV positive mothers are largely lost to follow-up.
"It is an
enormous frustration that we meet in our daily work."
More than
2.3 million children are living with HIV, the majority in sub-Saharan
Africa, where the disease has cut a swathe through poverty-stricken
populations.
Of these,
660,000 have an immune system that has been badly compromised by HIV,
exposing them to the risk of killer infectious diseases such as tuberculosis
and pneumonia.
MSF warned
that international agencies already battling AIDS have been late to spot the
devastating toll among infected children, and said if the situation is not
tackled soon, remedies will come too late.
Alongside
the warnings, MSF released two studies which showed good results among HIV
infected children treated with antiretroviral drugs.
The
potential benefits from such therapies however are limited, as pediatric
medicines are overpriced -- costing up to six times more than equivalent
drugs for adults, the agency said.
MSF said
treating children was fraught with challenges. Diagnosis is tough because
antibody-detection tests used for adults are inappropriate for newborns, and
test results take too long to process.
The lack of
pediatric doses means caregivers must split antiretrovirals used for adults
-- an imprecise method of treatment.
For
children who weigh less than 10 kilogrammes (22 pounds), even that strategy
will not work. The only treatment option is a syrup that the agency said is
difficult to measure, tastes bitter and often needs refrigeration.
"Sometimes
it is not possible to treat children in the villages because you can't
refrigerate a certain type of syrup, and the other one that does not have to
be refrigerated provokes anaemia," said Myrto Schaefer of MSF in
Australia.
"And then
you have a baby of less than three kilogrammes who already has anaemia, and
you can't give it to him!"
Adding to
the frustration is the fact that the drugs that do exist for children are
vastly overpriced.
"Because
the vast majority of infected children live in poor countries, most
pharmaceutical companies are hardly investing in developing pediatric
formulations," MSF said in a press statement.
Fernando
Pascual, an MSF pharmacist, said the price of some infant formulations is
reaching record levels.
Former US
president Bill Clinton, at the conference in his role as a campaigner on
issues including the AIDS epidemic, said he recognised the terrible plight
of HIV-infected children, and was committed to help alleviating it.
"I have
been despairing of this. I understood why the governments didn't spend money
on pediatric medicines, in the beginning it was more expensive and wide
swathes of young adults were dying," he told reporters.
Clinton
said several global governments had now recognised the problem, and were
devoting new funding to the plight of children.
"Pediatric
treatment has lagged behind other treatment woefully for the last few years,
given the change in funding priorities, it might actually jump ahead in the
next two years."
MSF
released data on Tuesday showing that given the right treatment, at the
right time, the youngest victims of the AIDS epidemic, which has killed 25
million people, can be saved.
Figures
showed that among 3,754 children under 13 years old in 14 nations, 80
percent were alive and continuing therapy after 24 months, with few adverse
side effects, and patients' immune systems were improving.
Cheaper generic from
India-based company could scuttle sales
A
Toronto company that has invested millions developing a new AIDS
medicine that is to be sent to Africa is now competing with another
drug firm that has created a cheaper version.
The
move by India-based Hetero Drugs means Apotex may struggle to find
buyers for Apo-triAvir, which has been hailed by agencies such as
Doctors Without Borders because it can be taken by pregnant women and
also helps prevent babies from contracting AIDS from their mothers.
Non-governmental organization Doctors Without Borders confirmed to the
Star that an India-based company called Hetero Drugs has
offered to sell the same amount of the newly created AIDS medicine for
about $15.8 million. Toronto's Apotex wants to charge more than $2
million more — $18.4 million — for the identical drug.
"Of
course, there's an irony to this," said Rachel Kiddell-Monroe of
Doctors Without Borders.
"What
happened was it took too bloody long here (Canada) to get the drug
approved."
Since
federal legislation was passed two years ago, not a single pill of any
generic drug has been sent to Africa or any other developing country.
The imbroglio has stoked criticism of the government, which this week
announced a formal review of the legislation.
Yet a
review may not be enough to save Apotex's drug, Apo-triAvir.
Apotex started working on the medication, which combines three drugs
in a single pill, in May 2005. The medication was submitted to Health
Canada last December for approval, which was granted in July.
Doctors Without Borders had agreed to pay 38 cents per pill for the
Apotex drug, which won't cover its $2 million-plus worth of research
and legal expenses so far, said Apotex president Jack Kay.
Hetero Drugs, which also makes generic versions of Tamiflu and the
anti-AIDS drug Viread, is offering the new AIDS medicine for 36 cents
per pill, which Doctors Without Borders would see administered twice
daily to as many as 60,000 patients.
Doctors Without Borders has agreed to buy 150,000 tablets of
Apo-triAvir from Apotex, contingent on the company receiving
permission to export it from either patent-holder GlaxoSmithKline or
Canada's Commissioner of Patents.
Pharmaceutical industry sources said it still might take years before
Apotex could navigate Canada's reworked drugs-to-Africa law. Kay,
who's been a dogged critic of Health Minister Tony Clement, said
Canada needs to decide whether it wants to scrap the legislation.
"Either
Canada wants to be a player here or it doesn't," he said.
But
it's not all bad news for Apotex. Besides aid agencies, the company
might also eventually sell Apo-triAvir to countries in sub-Saharan
Africa.
Tim
Gilbert, a Toronto lawyer who specializes in drug patent cases, said
he has contacted Apotex to offer help exporting the medicine to Ghana.
From there, he said regional trade treaties could be use to get
Apotex's drug to other developing nations. Using one country like
Ghana would help pare drug registration costs and other expenses.
HIV awakens a fighting spirit
Meet Musa "Queen"
Njoko. She's 34, the mother of a 14-year-old boy, a jazz singer, an
activist and a student at the University of South Africa. She also has
HIV.
She represents the
cusp of a discouraging trend in the AIDS pandemic: At least half of
all people living with the virus today are women. If current infection
patterns continue, women will soon outnumber men in the statistics.
For the Durban
resident, the virus has been, ironically, a kind of spiritual blessing.
It has meant a loss of innocence, but it has also drawn out great
personal strength.
"I am grateful to God
that he awakened the fighting spirit in my soul," Njoko said as she
took time out of her hectic schedule at the International AIDS
Conference in Toronto this week. "I didn't allow the outside world to
dictate how my life should be. I had my dreams, my aspirations, my
desires."
For the most part,
despite the disease, she has fulfilled them.
Njoko learned she had
contracted HIVwhen she was 22, in 1994. "It was an interesting time in
my country. It was the year we had our liberation (the end of
apartheid). It was a time when I was looking forward to positive
changes in my life. Then I was told I only had three months to live."
She had never even
heard of HIV.
Njoko got the virus
from her male partner, with whom she had already broken up.
"I didn't even know
how it was transmitted," she said.
Her son Thami was the
child of an earlier partner and is healthy.
Slowly, Njoko came to
terms with the news. In 1995, she became one of the first women — and
the first recording artist — in South Africa to disclose her
HIV-positive status.
Many people were
disgusted, embarrassed, or felt pity for her.
She relied on her
family for support and regularly performed as a jazz singer. She
recorded an album for Sony in 2000.
She became an
outspoken activist and established a wellness foundation that spreads
the word on the virus and helps women live with the disease. She also
heads Khanya AIDS Interventions, which develops AIDS policies for the
corporate sector, the government, women's groups and youth.
This week, her work
at the conference included appearing on a panel with Melinda Gates,
discussing women's rights and the need for women to take charge of
their own sexuality in the fight against the disease.
Stigma and
discrimination remain an issue for Njoko. She is careful to protect
her son from the outside world. He knows she has the virus, but she
doesn't take him with her when she speaks on HIV/AIDS.
Now, Njoko is
fulfilling another dream — she is just completing her first year
toward a commerce degree.
Legalizing sex trade touted to
cut HIVAs
Donna Summer moans "Love to Love You Baby" in the background, three
prostitutes are lolling provocatively across a satin-covered bed —
amid a scatter of sex toys — while half a dozen others sway to the
music nearby.
That this is
happening in the Metro Toronto Convention Centre — with plenty of the
city's finest patrolling the facility — is a little disconcerting on
first approach.
But there's a sharp
point to the scene, a highlight of the International AIDS Conference's
huge Global Village area.
"While it's meant to
be fun and humorous, we really did want to make this look like a
typical workplace," says Anna-Louise Crago, a prostitute and
spokeswoman for a Montreal sex-workers' alliance called Stella.
"This is exactly the
kind of setting we work in, " says Crago, who helped organize the
contingent of sex workers from 21 countries attending the conference.
Recognizing
prostitution as legitimate legal work, in both criminal law and labour
codes, is a key step to stamping out HIV and other diseases among sex
workers and the broader population, several researchers have told the
conference.
Prostitution remains
a main conduit for HIV in many parts of the developing world, and was
the focus of several research presentations.
Even former U.S.
president Bill Clinton came to the defence of sex workers Tuesday,
criticizing the Bush administration's ban on AIDS funding to groups
that don't officially oppose prostitution.
"I wish they would
just amend the law and say, `We disapprove of prostitution but here's
the money — go save lives,'" Clinton told a conference meeting.
"They are people, too,
and they deserve the chance to be empowered to save their lives. To me
it is a no-brainer."
Studies presented
this week urged countries to legally recognize sex workers, to improve
their safety and lower their susceptibility to AIDS.
"Sex workers are part
of the solution in the fight against HIV," says Crago. "And sex
workers need workers' rights and human rights in order to fight AIDS."
Many of the visiting
sex workers took to the streets around the conference centre yesterday
to voice their demands for legal recognition, which they say would
help combat the spread of AIDS by allowing prostitutes to come in from
the dark and marginalized areas — geographical and social — in which
they typically ply their trade.
Having legal rights
would provide the financial stability they need to refuse high-risk
encounters, and give them easier access to medical treatment and
education.
It would also reduce
their vulnerability to rape and sexual assault, lowering their chances
of contracting HIV, says Glenn Betteridge, a senior policy adviser
with the Canadian HIV/ AIDS Legal Network.
"In many countries
the law makes engaging in sex work illegal, and in those countries the
law disempowers women," Betteridge says.
"And we know, from
the history of the HIV epidemic, when women are disempowered they don't
have control over HIV prevention methods."
Betteridge said data
indicates that sex workers in Canada, who began to insist on condoms
and other protections early on in the AIDS crisis, don't pose a threat
as an HIV vector in this country.
In Southern Africa,
however, sex workers remain one of the most volatile links in the
spread of the disease.
Bangladesh worker angry at US
AIDS help restrictions
TORONTO -
A U.S. "loyalty oath" that aims to curb prostitution and prevent sex
trafficking has stymied one group's efforts to educate sex workers in
Bangladesh and left thousands of women without support, a local activist
said on Thursday.
Her eyes
filling with tears, Hazera Bagum said her group, Durjoy Nari Shangha, had
closed drop-in centers for sex workers in the Bangladesh capital in order to
win U.S. funding.
"This
feeling is like a broken heart, it's like a broken family," she said through
a translator at a news conference during the 16th International Conference
on AIDS in Toronto.
"All of
them are street workers. The only house they have is when they go to a
client for a few hours. Closing a drop-in center is like losing their homes,
like losing their meeting point, losing their school, losing everything."
The sex
workers collective -- its name translates roughly as "organization of women
who are hard to repress" -- had 20 drop-in centers before December, offering
sex and literacy education as well as moral support, toilets and a place to
wash and rest for up to 5,000 women.
It closed
them after signing what aid groups call the "prostitution loyalty oath" that
requires groups receiving USAID funding to have a policy opposing
prostitution and sex trafficking. The group now has just four centers,
geared to children and childrens' rights.
Bagum said
that before the centers closed, the group sold 73,000 condoms a month. That
has fallen to 30,000, even though health experts agree that condoms are the
best way of stopping the spread of AIDS.
A
spokeswoman for U.S. President George W. Bush's emergency plan for AIDS
relief said the U.S. plan targeted at-risk populations with "specific
outreach services, comprehensive prevention messages and condom information
and provision" and its ambassadors had visited many projects for high-risk
groups.
"Our office
has not received information that drop-in centers have closed, or that there
has been any interruption in services that target sex workers as a result of
our anti-prostitution policy," she said.
"Critics
who continue to spread misinformation about (the plan's) policies are
causing fear and confusion."
Some
organizations say they have chosen not to accept USAID funding rather than
compromise their positions, even though the locally available funding may be
far smaller than the amount available through the United States.
"We are
very proud of our decision," said Gabriela Leite, who works with eight local
sex worker organizations in Brazil.
"It's our
conviction that the sovereignty of our country should be respected."
Bangladeshi
community group working to educate sex workers in the country shared an
international award for its contribution toward prevention of HIV/AIDS.
The newly
launched Red Ribbon Award, announced at the 16th International AIDS
Conference in Toronto, was shared by four other groups from Ukraine,
Thailand, Zambia and Zimbabwe, the United Nations development agency UNDP
said in a statement on Friday.
Each of the
winners will receive $20,000 in prize money on World AIDS Day, on December
1, this year.
Blacks bear brunt
of AIDS in developed nations
TORONTO -
HIV infections are rising in black men and women living in developed nations
that have otherwise made strides against the disease, said participants at
the 16th International AIDS Conference in Toronto.
"AIDS in
America is a black disease no matter how you look at it, by gender or sexual
orientation or age or socioeconomic class or region in the country in which
you live," said Phil Wilson, executive director of the Black AIDS Institute,
at a press conference on Monday.
"Black
people bear the brunt of this epidemic."
People of
African and Caribbean descent -- particularly heterosexual women and men who
have sex with men -- have higher HIV infection rates than the overall
population in developed countries like Canada and the United States, said
conference participants.
Blacks make
up 13 percent of the United States population, but represent an estimated 42
percent of people living with HIV/AIDS. Ontarians of African and Caribbean
descent make up less than five percent of the population but account for 14
percent of those with HIV/AIDS and 19.5 percent of new infections in 2004 in
Ontario, a rise of 82 percent in five years. Their HIV infection rate is
almost 13 times the overall rate.
AIDS is the
leading cause of death for African American women aged 25 to 34, and in
2003, 60 percent of all American females living with HIV/AIDS were black.
African American women make up 68 percent of new HIV cases in the U.S.
"If we, as
black women, in America do not decide today and every day that AIDS is our
face and fight, in 2020 there'll be no black women in America," said Grazell
Howard, first vice president of the National Coalition of 100 Black Women.
A study
released by the Centers for Disease Control in June 2005 showed that black
men who have sex with men in the United States had HIV infection rates
higher than in sub-Saharan Africa, at 46 percent
Another CDC
study presented at the conference showed that while American high school
students were overall engaging in less sexual behavior that put them at risk
for HIV infection since the early 1990s, decreases in sexual intercourse and
increases in condom use in African American teenagers leveled off over the
past few years, after progress throughout the early 1990s.
The study's
findings showed that there may be a need to intensify prevention efforts in
black and Hispanic adolescent populations in the United States, said Dr.
Laura Kann of the CDC.
It's not
only in the developing world that people die due to lack of access to
treatment, said the Canadian Treatment Action Council. In the conference's
host country, a variety of barriers stand in the way of treatment for
HIV-positive immigrants, said Esther Tharao of the council.
Stigma --
both in the general population and their own cultural communities -- makes
it hard for vulnerable populations to get care. Immigrants and refugees
without residency status in Canada don't qualify for the country's public
health care, and they face further difficulties due to differences in
culture and language.
"We need a
Canadian strategy to support communities from countries where HIV is endemic,
and we need funding to make it work," said Tharao in a statement.
Several
conference activities focused on mobilizing populations of African and
Caribbean descent in the fight against HIV.
"For too
long, our community has sat idly by as this epidemic has ravaged our
families and claimed the lives of our brothers and sisters," said Cheryl
Cooper, executive director of the National Council of Negro Women.
"We need to
make some noise. Everyday, everywhere we need to start by saying, I am
fighting against HIV. If we take to the streets and the churches and we use
all these platforms, we can beat this," said Maxine Waters, a Representative
from California.
AIDS researcher slams South
Africa's inaction, world's silence
TORONTO -
A leading AIDS activist and researcher slammed the government of South
Africa on Thursday for failing to take strong measures to stem the spread of
HIV in that country - and lambasted political leaders elsewhere for not
calling South Africa on its failures.
Mark
Heywood, whose remarks drew a rousing response from an audience at the
International AIDS Conference, also warned that a similar pattern of
political avoidance could lead to an explosion of HIV cases in China, where
UNAIDS has warned 10 million new infections could occur by 2010.
"When this
number of people are dying in the face of anti-leadership and denial, then
the world has to speak up," insisted Heywood, senior researcher and head of
the AIDS Law Project at the University of the Witwatersrand, South Africa.
"There's a
terrible silence by political leaders outside of South Africa. Bill Clinton
can't get it out of his mouth to criticize Thabo Mbeki. Kofi Annan can't
criticize Thabo Mbeki and the South African government. If there's this
silence, then the crisis for us will go on and on and on. "
Mbeki, the
South African president, long denied that HIV is the cause of AIDS and
blocked the import of the antiretroviral drugs that have turned AIDS from a
killer to a chronic illness for many infected people living in countries
where the drugs are available. He and Stephen Lewis - UN Secretary General
Kofi Annan's special envoy for AIDS in Africa - have butted heads so often
that Lewis has been barred from undertaking his work in that country.
An
estimated 5.5 million people in South Africa - a country of 47.5 million -
are infected with HIV and roughly 800 people a day die from AIDS there.
Heywood
said that while scientists have succeeded in developing tools to fight the
transmission of HIV and blunt the virus's assault on the immune systems of
those infected, a lack of political leadership is preventing the benefit of
those advances from being fully realized. For instance, only 17 per cent of
the people with AIDS who need antiretroviral treatment are receiving the
drugs, he said.
"Governments
have power. And governments have a responsibility to put those advances into
place," said Heywood, who also noted that while the world knows how to
prevent mother-to-child transmission of HIV, too many infants are still
being born with the virus.
He incited
delegates to the conference to demand political leadership. And he insisted
that by the end of this year the United Nations should set firm targets for
reduction of mother-to-child transmission and for delivery of antiretroviral
drugs to those in developing countries who need them.
"Behind us
are 40 million people (living with HIV-AIDS) who can't come and stay in posh
hotels and walk the streets of Toronto," Heywood said.
"We have a
responsibility to them."
Heywood
also called for the resignation of Dr. Manto Tshabalala-Msimang, South
Africa's controversial minister of health.
Tshabalala-Msimang promotes nutrition and natural remedies as key weapons in
the fight against HIV-AIDS, promoting lemons, garlic and beet root as
treatments. She has drawn criticism - and protesters - at the Toronto
conference for using South Africa's booth in the exhibition hall to promote
her ideas.
Heywood
suggested tens of thousands of South African lives could have been saved had
the country made a concerted effort to fight transmission of HIV.
Heywood
warned that China experiences many of the same social problems that fuelled
the transmission of HIV in South Africa and he questioned whether the global
community would raise its voice to ensure that the 10 million new cases
UNAIDS projects for the country won't come to pass.
Current
official estimates set the number of HIV infections in China at 650,000. But
UNAIDS believes that number could explode over the next four years.
"That can
be stopped but it can only be stopped if the Chinese government mounts the
necessary political will and works with civil society in order to stop that
epidemic," Heywood said.
A Chinese
delegate to the conference challenged Heywood's assertions from the floor,
inviting him to come to China to see the situation for himself. The delegate
suggested Heywood's comments about sex workers being jailed and other
at-risk groups being further jeopardized by government policies weren't well
informed.
Heywood
countered, though, that the Chinese government is still jailing AIDS
activists and perpetuating other human rights violations that undermine the
fight against HIV.
Political leaders accused of AIDS
genocide
“If you have evidence your
inaction is responsible for millions of deaths, you promise to correct that
situation, then you fail to deliver, what do you call that?” Julio Montaner
said in an interview.
“It's not
ignorance. It's not mere negligence. It's more than a crime against humanity.
“It can
only be characterized as genocide.”
Dr.
Montaner, director of the B.C. Centre for Excellence in HIV/AIDS in
Vancouver and one of the world's leading AIDS researchers, said that
life-extending drug cocktails must be made available to everyone in the
world who is infected and would benefit, regardless of the cost.
“These
drugs are so powerful that we have a moral imperative to make them available,”
he said.
There are
an estimated 38.6 million worldwide living with HIV/AIDS, according to the
United Nations agency UNAIDS. According to data presented at the 16th
International AIDS Conference, 1.6 million people are getting antiretroviral
drugs in developing countries and as many again in the developed world.
Worldwide,
only 21 countries (including Canada) are providing the treatment to at least
half of patients who could benefit.
“These are
unacceptable levels,” said Cristina Pimenta, the former head of the
prevention unit of the Brazilian National AIDS Program. “We are moving
backwards every day.”
What she
means is that the number of new infections — 4.1 million last year — is far
outpacing the number being newly treated.
Similarly,
the cost of treatment and prevention is significantly higher than the
spending commitment of governments.
Last year,
an estimated $8.7-billion was spent on HIV/AIDS, about half of what is
required to provide basic treatment, prevention and care.
Providing
drug cocktails to everyone would cost an estimated $7-billion annually, and
as much again for related testing and health care.
Mark
Heywood, national secretary of the Treatment Action Council in Johannesburg,
South Africa, said that the failure to provide treatment to people with
HIV/AIDS should be a violation of fundamental human rights.
“We have
the means, so what stops us from acting?” he said. “And what should be done
about those in power who refuse to act? These are the most pertinent
questions facing the next stage of the AIDS epidemic.”
Mr. Heywood
said vague promises to act are not enough, that the United Nations must, by
year's end, set firm targets for delivery of antiretroviral drugs and
reduction of mother-to-child transmission of the disease.
He also
called on delegates to hold politicians' feet to the fire to ensure they
deliver.
Previously,
the United Nations vowed to get AIDS drugs to three million by the end of
2005. They fell short of that target, in large part because countries like
Canada failed to come through.
Two years
ago, Canada adopted legislation becoming the first Group of Eight country to
allow generic pharmaceutical companies to export life-extending medicines to
developing countries that don't have the capacity to manufacture drugs
themselves, but not a single pill has been delivered.

Rapid tests mean more learn HIV
status
Rapid HIV
tests lead to more people getting tested and receiving their results,
according to a study by the US Department of Veterans Affairs presented at
the 16th International AIDS Conference.
Both
traditional testing and newer rapid tests were likely to result in higher
screening rates for HIV, according to the study. But patients who received
rapid testing were much more likely to learn their results.
HIV testing
is cost-effective, but testing rates for at-risk populations in the U.S. are
low. "Even people who are in care and are seeing their doctor on a regular
basis, and are identified as being at risk for HIV infection, are not being
tested at nearly the rate that they should be," said Dr. Henry Anaya, who
presented the study.
Testing is
important because people tend to reduce their risk behaviors when they know
their HIV status, Anaya said.
Patients
waiting for an appointment at VA primary/urgent care clinics in Los Angeles
were randomly split into three testing groups. The patients were all between
18 and 65 years of age and were unaware of their HIV status. None had been
tested in the past year.
The first
group of patients was prompted to ask their doctor for an HIV test during
their appointment; the second group was referred to a nurse for traditional
HIV testing; and the third group was also referred to a nurse but these
patients received the rapid HIV test.
Traditional
HIV testing involves two appointments -- one for testing, and another some
days later, to receive the results and counseling. Rapid tests involve an
oral swab or a finger stick and results can be available in as little as 20
minutes.
Forty-one
percent of the patients told to ask their physician for a test actually did,
and 41 percent of those tested received their results. Double the patients
who were referred to a nurse for testing actually did take the HIV test.
Eighty-four percent of those referred for traditional testing received it,
as did 93 percent of those in the rapid test group.
But many
more patients in the rapid test group actually received their results -- 90
percent compared to 52 percent for those who had to return to get their
results and counseling.
"The
magnitude and direction of these results surprised even us," Anaya said.
The results
show that referring patients for testing is effective in both cases, but
rapid testing resulted in nearly double the patients ultimately learning
their HIV status.
The testing
project is currently being used in an outreach effort directed at homeless
veterans with the Los Angeles County, and the hope is for it to be expanded
nationally across the Department of Veterans Affairs, Anaya said.
Brazilian designer: condoms,
basic as jeans, necessary as love
Thousands of condoms pile in
the corner. Buckets of paint lie on the shelf. She cuts, twists, shapes, melts,
pastes, colors, crochets and sculpts, with her fingers and nails stained black.
365 hours later, a colourful elegant gown made of 6,500 condoms debuts.
Adriana Bertini,
a Brazilian artist living in São Paulo, uses expired or defective condoms as raw
material to make pieces of art. Her creations include ornate evening dresses,
vivid bikinis, elegant shawls, flowery carnival costumes, and other plastic arts.
"I want my art
to be visible everywhere, reminding people of the necessity of HIV prevention"
Bertini says. “I prefer working more with the figurines, because I noticed that
they make people think about the meaning of ‘Wear against AIDS’.”
Bertini started
her career at Brazil's fashion houses, and made her first dress from condoms in
1997. Since then, the designer has made around 200 sculptures, 80 tapestries and
160 figurines from condoms. The most condoms she has ever used on a gown -
around 80 thousand - was on one wedding dress.
"My idea is to
promote condom use not as a commercial fashion but as a conceptual fashion, be
it conscious or subconscious. The idea is to wear them at the right time, not
just as a trend, on clothes" says Bertini.
Bertini started
working in HIV prevention in 1994, after she spent time with HIV positive
children as a volunteer for GAPA, an HIV prevention group. "In the beginning, I
worked with condoms but not necessarily in the context of AIDS," the designer
says "The AIDS issue came along with my work with children living with HIV. I
realized that I could use fashion for AIDS awareness."
“I volunteered
to do the HIV prevention work,” says Bertini, who at the time did not know
anyone living with HIV. “Then I made friends who were HIV positive and this
stimulated me even more to promote prevention. Today, I have already lost some
dear people to AIDS. I think this is the minimum I can do, being a conscientious
person faced with a problem of this magnitude. ‘If you have conscience, act'.”
Bertini’s
designs can be seen at fashion shows and in magazines, or are exhibited in
museums. “The focus is not on wearing my gowns, but on introducing condoms into
everybody’s lives, breaking taboos and giving the public a chance to ponder.”
While Bertini’s
designs are often shown in Brazil, she has also had important international
exposure. Her work was exhibited at the International AIDS Conference in
Barcelona, Spain, in 2002, and at the 15th International AIDS Conference in
Bangkok, Thailand, in 2004, among others. She has also proposed an exhibit in
the cultural programme of the 16th AIDS Conference in Toronto this coming August:
“I am waiting for the selection to be finalized.”
Reactions of
the public to her designs vary. Some people whisper about it, others laugh or
dismiss it as inappropriate, and then there are those who want to meet her and
tell her their problems.
“There a lot of
parents who want to thank me because it was through my art that they’ve reached
out to their children to talk about sexuality,” she says.
All her
material comes from condom manufacturers, and the proceeds from the sales of
dresses - prices range from $700 to $5,000 - go directly to organizations
involved in the fight against AIDS. Bertini and her HIV-positive apprentices do
not make their living directly from their work, but instead rely on sponsors.
"I'm not doing
this to make money but rather as a social act, as art aimed at others. I hope
that by using condoms to create something new, I can inspire reflection, foster
discussion, and challenge taboos." says Bertini who is quickly becoming
well-known in international activism circles.
The 34 year-old
was awarded with the Nkosi Johnson Community Spirit Award in 2004 by the
International Association of Physicians in AIDS Care, Washington DC, (IAPAC) in
recognition of her 10 years of artistic activism. "You understand, condoms must
become as basic as a pair of jeans and as necessary as a great love," Bertini
emphasizes.
Closing ceremonies at AIDS conference:
Time to deliver, Stephen Lewis says
TORONTO - World
governments were exhorted Friday to step up to the plate and deliver on funding
promises and the social change needed to stop spread of HIV-AIDS and provide
lifelong treatment for current sufferers, regardless of their ability to pay.
The clarion
calls came during the closing session of the week-long International AIDS
Conference, the 16th such gathering of scientists and activists since the early
days of the AIDS pandemic.
Stephen Lewis,
the UN Special Envoy for AIDS in Africa, delivered an oratorical barn burner in
which he excoriated the government of South Africa, slammed the G-8 countries
for not living up to AIDS funding promises and insisted the tragic spread of HIV
cannot be stemmed until gender inequality is righted.
Lewis - whose
term concludes at the end of this year and whose hard-hitting remarks were
greeted with sustained and reverential applause - admitted that in the battle
against AIDS, the factor that makes him feel "most enraged" is the inequality of
women and how that puts them at high risk of becoming infected.
Expansion of
programs to deliver life-saving HIV drugs to those in need in developed and
developing countries is growing at a moderate rate, he suggested. But the costs
of striving towards universal access for all in need are enormous and it is not
clear where the funds will come from.
"We are on the
cusp of a huge financial crisis," Lewis warned the gathering, noting that the
G-8 countries haven't lived up to the pledging promises they made to the Global
Fund for AIDS, Tuberculosis and Malaria at their 2005 summit in Gleneagles,
Scotland.
"No one is
asking for any more than was promised," Lewis said. "Everything in the battle
against AIDS is being jeopardized by the G-8."
The Canadian
government, which has been roundly criticized at this conference for Prime
Minister Stephen Harper's refusal to take part in the opening ceremony, got off
relatively lightly in the ceremonies marking the close of the conference, which
drew an estimated 30,000 scientists, activists, journalists and representatives
of aid agencies to Toronto.
Conference
co-chair Dr. Mark Wainberg, director of the McGill AIDS Centre in Montreal, said
that while he lamented Harper's absence, he felt grateful to live in a country
where one can criticize political leaders. As he mentioned Harper's absence,
calls of "shame" rang out through the assembly.
Wainberg
obliquely opened the attack on South Africa, where the government of President
Thabo Mbeki has confounded and enraged the scientific and public health world by
initially denying the link between HIV and AIDS and then resisting the use of
antiretroviral drugs. Mbeki's health minister, Dr Manto Tshabalala-Msimang,
promotes the use of lemons, garlic and beet root as treatments for AIDS.
"We recognize
the problem that is sadly posed by HIV denialists," said Wainburg. "It is
correct to ask how many additional millions of HIV cases are attributable to the
failure of certain world leaders to directly and honestly address issues of
HIV-AIDS with their people."
But Lewis named
names. "South Africa is the unkindest cut of all."
"It is the only
country in Africa whose government continues to propound theories more worthy of
a lunatic fringe than of a concerned and compassionate state," he said, noting
between 600 and 800 people a day die of AIDS in South Africa.
"The government
has a lot to atone for. I'm of the opinion that they can never achieve
redemption."
Lewis, who has
been barred from functioning for the UN in South Africa because of his
opposition to the government's positions, admitted he has been told that as a UN
representative he should not be publicly critical of a member state.
"It is not my
job to be silenced by a government when I know that what it is doing is wrong,
immoral and indefensible."
|